Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
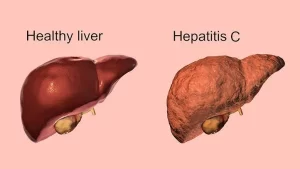
Hepatitis D is a kind of viral hepatitis caused by the hepatitis delta virus (HDV), HDV is one of five known hepatitis viruses: A, B, C, D, and E, HDV complications such as liver failure in acute infections and a rapid progression to liver cirrhosis, with an increased risk of developing liver cancer in chronic infections, In combination with the hepatitis B virus, hepatitis D has the highest fatality rate of all the hepatitis infections.
HDV
Hepatitis D is also known as “delta hepatitis,” It is a liver infection caused by the hepatitis D virus (HDV), Hepatitis D only takes place in people who are infected with the hepatitis B virus.
- RNA virus.
- Blood borne infection.
- Coinfection with acute HBV infection or as a superinfection in patients with Pre-existing chronic HBV infection.
- Incubation period: 1 to 4 months.
- Diagnosis: anti-HDV Abs (IgM, IgG) & HDV RNA.
- Treatment: Pegylated interferon 48 weeks.
HCV
- RNA virus.
- Blood borne.
- 7 genotypes.
- Incubation period: 15 to 150 days.
- Acute cases are usually asymptomatic.
Acute HCV
The classic diagnosis of acute HCV:
- The patient comes with acute hepatitis.
- HCV-RNA is positive.
- Anti-HCV is negative.
Spontaneous clearance
- Of persons recently infected with HCV, approximately 27% clear infection spontaneously.
- Predictors of spontaneous clearance: Symptomatic patients (jaundice), IL28B CC genotype.
Treatment of acute HCV
- Monitoring for Spontaneous Clearance: All patients with acute HCV should have.
- HCV RNA monitoring every 4 to 8 weeks for a minimum of 16 weeks. (6 months).
- If the decision is made to treat a patient with acute HCV infection, the same regimens should be used as recommended for the initial treatment of patients with chronic hepatitis C.
Factors that accelerate the progression
- Male gender.
- Older age at infection.
- Duration of infection.
- Alcohol use.
- Insulin-resistant diabetes mellitus.
- Steatosis.
- HIV infection and other immunosuppressive states.
Treatment of chronic HCV
Drugs:
- Interferon (regular, pegylated).
- Ribavirin.
- DAAs (protease inhibitors, polymerase inhibitors, NS5A inhibitors).
Key Data for HCV treatment decisions:
HCV treatment history:
- Interferon and ribavirin regimen?
- Protease inhibitor? Sofosbuvir?
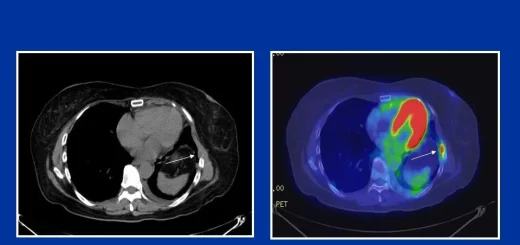
Fibrosis stage? Options for fibrosis assessment.
Drugs
- Sofosbuvir (Sovaldi).
- Simeprevir (Olysio).
- Daclatasvir (daklinza).
- Paritaprevir/ritonavir Ombitasvir (Qurevo).
- Sofosbuvir + Ledipasvir (Harvoni).
- Sofosbuvir + velpatasvir (epclusa).
General rules
- The treatment duration is 3 to 6 months.
- Drug combinations using different groups are given, and monotherapy is contraindicated.
- The response rate is generally > 90%.
- Sofosbuvir cannot be used in severe renal impairment.
- Protease inhibitors cannot be used in decompensated cirrhosis.
Extra-Hepatic Manifestation
- Mixed cryoglobulinemia.
- Non-Hodgkin lymphoma.
- DM, type II, and insulin resistance.
- Cardiovascular disease.
- Fatigue.
- Cognitive impairment.
- Reduced health-related quality of life.
- Renal disease.
Mixed cryoglobulinemia
- Is a systemic vasculitis caused by the deposition of circulating immune complexes in the small vessels.
- Characterized by the presence of circulating Igs that precipitate at low temperatures.
- (under 37 °C) and can solve by serum re- warming.
- Type II (MC-II):(Polyclonal IgG and monoclonal IgM with rheumatoid factor (RF) activity.
- Patients with joint pain and positive rheumatoid factor may be true rheumatoid arthritis or chronic HCV with mixed cryoglobulinemia.
- We differentiate between them by Anti-CCP which is positive in rheumatoid arthritis and negative in chronic HCV with mixed cryoglobulinemia.
Clinical picture
- The most common symptoms are weakness, arthralgias, and orthostatic palpable purpura (Meltzer and Franklin triad).
- Peripheral neuropathy represents the most frequent clinical feature after the triad, followed by sicca syndrome & renal involvement.
Lab
Serum-mixed CGs, high RF values, and reduced C4 values are the most frequent laboratory data.
Treatment:
Antiviral therapy is considered, when feasible, the mainstay of treatment for most HCV-linked extrahepatic diseases.
Occult hepatitis C (OCI):
- Elevated transaminases.
- – ve HCV antibodies.
- +ve HCV RNA in low levels detected by Amplification techniques in: Serum, PBMCs (Peripheral Blood Mononuclear Cells), and liver biopsy.
A patient with HCV
HCV-RNA is positive and Anti-HCV is negative and the patient is known to have hepatitis C, in this case, we have different possibilities:
- 1. The patient is in the acute stage (high transaminase more than 10 times upper normal).
- 2. The patient is in occult hepatitis C (the enzymes will be much less as it is a form of chronic hepatitis C).
HEV
- RNA virus, 8 genotypes.
- Only G 1-4 infect humans. IP 15-60 days.
- Acute infection is usually silent & self-limited.
- <5% may develop symptoms of acute hepatitis, Jaundice mainly cholestatic (in 90% to 100% ).
- Progression to ALF is rare, particularly with pregnant women.
- Diagnosis by HEV Abs IgM & HEV RNA.
- In immunocompromised patients, PCR is the most reliable test for diagnosis because serologic testing may be negative.
- Acute HEV infection does not usually require antiviral therapy. Most infections are spontaneously cleared.
- Ribavirin ( 600 mg/day) for 3-6 months in acute severe & chronic cases.
Extrahepatic manifestations
- Meningitis.
- Neuralgic amyotrophy.
- Guillain-Barre syndrome.
- Cryoglobulinemia.
- Glomerulonephritis.
- Myocarditis.
- Pancreatitis.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Histological structure of gallbladder & Pancreas, Functions of the liver & Composition of bile
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Liver development, congenital anomalies, function & Pancreas development