Vascular Liver Disorders, Causes and risk factors of Budd-Chiari syndrome
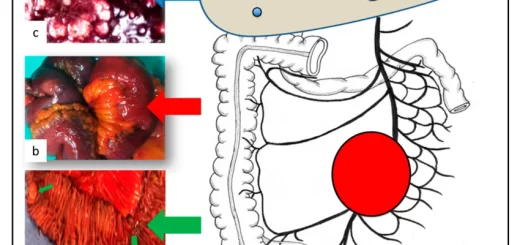
The liver has a unique blood supply as it has: 2 feeding blood vessels (portal vein & hepatic artery). 3 vessels draining in one large vessel as an outlet. If any of these vessels or other small vessels are affected, this is called vascular liver disease. The portal vein supplies the liver with 70% of its blood supply and it drains the whole GIT as it takes the venous drainage of GIT and enters it into the liver.
Vascular Liver Disorders
The portal vein carries the deoxygenated blood to the liver, The hepatic artery carries the oxygenated blood to the liver, the hepatic artery supplies the liver with 30% of its blood supply. The liver doesn’t have capillaries but has sinusoids, The sinusoids collect and drain the venous blood of the liver into 3 veins (right, left, and middle hepatic veins) then drain later into the IVC, The most important vascular liver diseases that we will focus on is Portal vein thrombosis and Budd-Chiari syndrome.
Vascular Diseases of the liver
- Budd-Chiari syndrome.
- Portal vein thrombosis.
- Hepatic artery diseases (aneurysm, thrombosis).
- Sinusoidal obstruction syndrome.
- Radiation-induced liver disease.
- Peliosis hepatis and sinusoidal dilatation.
- Congenital vascular malformations.
Budd-Chiari syndrome
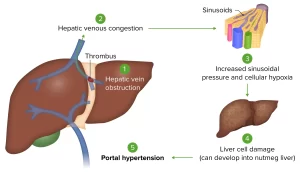
Budd-Chiari syndrome means occlusion of one or more of the hepatic veins with or without occlusion of the IVC or occlusion of the IVC alone without the hepatic veins. Obstruction was in the hepatic veins (62%) and IVC (7%) of the cases. The disease differs according to the occlusion if it is:
- Complete or partial.
- Rapid or slow.
- The nature of occlusion.
Most common in:
- Budd-Chiari syndrome is more common in women.
- In the third or fourth decade of life.
- It is more associated with females in their pregnant state which means during pregnancy.
- It has an association with the means of oral contraceptive pills.
- Most common symptoms are ascites (84%) and hepatomegaly (76%) of the cases.
- The myeloproliferative disorder is present in 23% of the cases (polycythemia vera).
Major causes of the Budd-Chiari Syndrome
The nature of the occlusion may be
- Thrombus: Fibrin threads and platelets between them, This normal thrombus and it is the most common cause of occlusion.
- Malignant thrombus: Extension of malignant tumors.
- Inflammation of the blood vessel.
The causes and risk factors are:
- Malignancy (Hepatocellular carcinoma).
- Infections and benign lesions of the liver.
- Oral contraceptives.
- Pregnancy.
- Myeloproliferative diseases.
- Hypercoagulable state (penicillin thrombophilia-protein C deficiency- protein S deficiency).
- Behcet’s disease (Affect the intima of the blood vessel and cause vasculitis (inflammation of the vessel)}.
- Membranous webs of IVC.
- Idiopathic.
Congenital anomalies may be found in one of the hepatic veins or especially in the IVC in the form of a membrane or web and this is common in the far east and all these congenital anomalies are idiopathic we don’t know the cause.
Examples of thrombophilia (hypercoagulable state) that may be associated with the thrombosis of one of the venous drainage of the liver: or generalized (systemic) causes of portal vein thrombosis (or one of its branches right or left):
- Myeloproliferative disorders.
- Antiphospholipid syndrome.
- Paroxysmal nocturnal.
- Hemoglobinuria.
- Behçet’s disease.
- Factor V Leiden mutation.
- Factor II mutation.
- Protein C deficiency.
- Protein S deficiency.
- Antithrombin deficiency.
- Plasminogen deficiency.
- Recent pregnancy.
- Recent oral contraceptive use.
- Hyperhomocysteinemia.
- TT677 MTHFR genotype.
Clinical presentation
- If the occlusion is slow and partial, this ischemia provokes and allows the formation of new blood vessels (collaterals) and these collaterals maintain the venous drainage or the patency of the part of the vessel that has been occluded.
- If good collaterals formation happens, the patient will present late as subacute or chronic as he will not have acute symptoms because the circulation has been maintained with the help of collateral circulation.
- If the occlusion is rapid or nearly complete, the patient will come with acute symptoms (rapidly accumulating ascites or rapidly formed jaundice or coma and acute liver failure).
- In the subacute state, the duration of occlusion is usually less than 6 months so the cirrhosis wouldn’t have been formed yet.
- Collaterals are blood vessels that bypass the site of obstruction as they begin under the site of obstruction and form side branches or shunts and end in the post-obstruction site.
A. Acute (20%)
- 2% with fulminant hepatic failure.
- Most commonly in women (during pregnancy).
Clinical picture
- Pain in the right upper quadrant and hepatomegaly and the liver may be tender on examination.
- Jaundice and ascites develop rapidly.
- These signs and symptoms don’t have to happen together.
- Liver function can deteriorate quickly (hyperglobulinemia-high transaminase – disturbed synthetic function and this is a sign that the patient is about to have a liver failure), leading to hepatic encephalopathy.
Differential diagnosis
- ischemic, viral, malignant/infiltrative, and toxic hepatitis.
- Other causes of acute fulminant liver failure.
B. Subacute (40%) & Chronic (40%)
- Subacute: having signs or symptoms, for < 6 months and no evidence of cirrhosis.
- Chronic: having signs or symptoms for > 6 months with evidence of cirrhosis.
Clinical manifestations
- Depend upon the extent of occlusion, and the recruitment of collateral circulation.
- Chronic occlusion of the hepatic veins may be associated with hypertrophy of the caudate lobe
- Because the caudate lobe has a venous drainage separate from the other 3 hepatic veins as it drains directly to the IVC, so if one or the 3 hepatic veins have been occluded, compensatory hypertrophy will happen in the caudate lobe to compensate the shrinkage or atrophy in the other lobes that drain in the other 3 hepatic veins, so the caudate lobe will compensate the function of the whole liver).
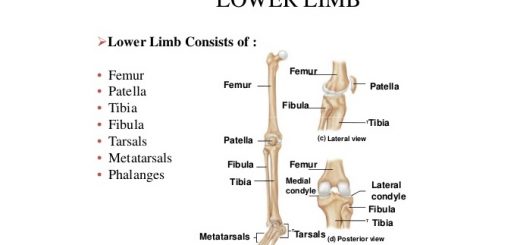
- This causes compression of the intrahepatic portion of the IVC, leading to lower extremity edema.
- The patient will come chronic which means cirrhosis and its manifestations whether compensated or decompensated.
- The chronic patient will maybe present with ascites or jaundice or hepatomegaly or upper GIT bleeding due to the formation of esophageal or gastric varices or hepatic encephalopathy or even hepatocellular carcinoma (HCC).
You can subscribe to science online on Youtube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Autoimmune Hepatitis symptoms, types, diagnosis, causes and treatment
Primary biliary cirrhosis symptoms, cause, diagnosis, treatment, and Osteoporosis
Diagnosis of the cause of jaundice, Hepatobiliary imaging, treatment of cholestasis and Pruritus
Liver Cholestasis types, causes, features, symptoms, diagnosis, and treatment
Conjugated hyperbilirubinemia cause, symptoms and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer