Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption and secretion
The urinary system consists of the kidneys, ureters, bladder, and urethra, It eliminates the waste from the body, It is known as the renal system or Urinary tract, It regulates the blood volume and blood pressure, It can control levels of electrolytes and metabolites, and regulate blood pH.
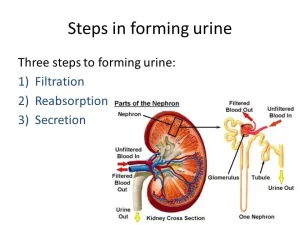
Urine formation
Urine is formed in the kidneys through the filtration of blood, and it is passed through the ureters to the bladder, where it is stored, the urine is passed from the bladder through the urethra to the outside of the body during urination, Urine is formed by 3 main processes:
- Glomerular filtration.
- Tubular reabsorption.
- Tubular secretion.
Glomerular Filtration
Glomerular filtration is the first step in urine formation, The glomerulus acts as a filter between the blood and the tubule, The glomerular capillary membrane has high permeability and is estimated to be 100-500 times the permeability of a usual capillary, The glomeruli act as simple filters, and this filtration is a passive process.
The driving force of this filtration is the high capillary blood pressure in the glomeruli, The fluid that filters through the glomeruli into Bowman’s capsule is called “glomerular filtrate”, This filtrate is nothing but plasma minus its colloids (fats, proteins), thus all substances with a molecular weight above 70.000 Daltons (Da) do not pass through.
Dynamics of glomerular filtration
- Glomerular pressure: the glomerular pressure is about 60 mmHg.
- Pressure in Bowman’s capsule: pressure in the capsule is about 18 mmHg.
- Colloid osmotic pressure in the glomerular capillaries: Approximately one-fifth of the plasma in the capillaries filters into the capsule, thus the protein concentration increases about 20 percent as the blood passes from the arteriolar to the venous ends of the glomerular capillaries, If the normal colloid pressure of blood entering the capillaries is 28 mmHg, it rises to approximately 36 mmHg by the time the blood reaches the venous ends of the capillaries, and the average colloid osmotic pressure is about 32 mmHg.
Filtration pressure (FP): it is equal to the glomerular pressure minus glomerular colloid osmotic pressure and capsular pressure. Therefore, FP = 60 – (32 + 18) = 10 mmHg.
The filtration coefficient (Kf)
It is the glomerular filtration rate for both kidneys per mmHg of filtration pressure. Therefore, the glomerular filtration rate is equal to the filtration pressure X the filtration coefficient, i.e.GFR Filtration pressure X Kf. The normal filtration coefficient is 12.5 ml per minute per mmHg of filtration pressure: GFR = 10 x 12.5 = 125 ml/min.
180 liters are filtered per day. As plasma volume is about 3 liters, plasma is filtered by kidneys 60 times a day. The high rate of glomerular filtration is due to:
1. The high capillary blood pressure, higher than any other capillary in the body, due to the special arrangement of the renal arterial system:
- Renal artery is short, wide, and arises directly from the aorta, this leads to high pressure in the afferent glomerular arteriole.
- The afferent glomerular arteriole is wider and shorter than the efferent arteriole; this creates a high glomerular capillary pressure which causes filtration of fluid through the capillary membrane.
2. The high glomerular filtration coefficient which depends upon:
- The surface area of the filtering membrane.
- The permeability of the filtering membrane. The total surface area of the filtering membrane is 2 square meters. The permeability of the filtering membrane is very high. Thus, the high GFR can be accounted for by high hydrostatic pressure forcing through a large membrane with high permeability.
Factors affecting glomerular filtration rate
1. Renal blood flow (RBF)
An increase in the rate of blood flow through the nephrons greatly elevates the glomerular pressure and increases the glomerular filtration rate. Normally, a very large amount of plasma is filtered through the glomerular membrane; thus the colloid osmotic pressure in the glomerulus rises very high and opposes further filtration because of the retained colloids. Filtration stops until new plasma flows into the glomerulus; consequently the greater the rate of plasma flow in the glomerulus, the greater is the filtration rate.
2. Diameter of glomerular blood vessels
Afferent glomerular arteriole
- The arteriolar constriction decreases the rate of blood flow into the glomerulus, decreases the glomerular pressure and thus, decreases the filtration rate.
- Arteriolar dilatation increases the glomerular blood flow and glomerular pressure both effects increase the filtration rate.
Efferent glomerular arteriole
- Arteriolar dilatation lowers the glomerular pressure and decreases the filtration rate.
- Arteriolar constriction: mild constriction increases the glomerular pressure and increases the filtration force; severe or moderate constriction decreases the glomerular flow rate and decreases the filtration rate, The plasma will remain for a longer period in the glomerulus, and extra-large amounts of plasma will filter out, This increases the plasma colloid osmotic pressure and a paradoxical decrease in GFR occurs despite the increase in glomerular pressure.
3. Sympathetic stimulation
During sympathetic stimulation eg. stress conditions, the afferent arterioles are constricted, both renal blood flow and filtration decrease. With very strong stimulation, the glomerular flow and pressure are reduced so greatly that the urinary output can fall to zero.
4. Arterial blood pressure
An auto-regulatory mechanism prevents a significant rise in the glomerular pressure corresponding to a rise in systemic blood pressure, Automatic afferent arteriolar constriction occurs in case of high arterial pressure, However, the glomerular filtration rate increases only a few percent if the increase in blood pressure is not severe.
5. Intrapelvic pressure
A rise of pressure in the renal pelvis will produce back pressure in the intracapsular pressure which antagonists the filtration force. A pressure higher than 28 mmHg will stop the filtration and consequently urine formation e.g. renal pelvic stone or tumors.
6. Colloid osmotic pressure
The colloid osmotic pressure of plasma proteins antagonizes filtration. Hypoproteinemia will increase the filtration rate.
7. Permeability of glomerular capillaries
Increased permeability of glomerular capillaries increases the GFR The permeability of the glomerular capillaries and Bowman’s capsule is absent for substances of molecular weight higher than 70,000 Da. In the case of plasma proteins, the serum albumin has a molecular weight of 70.000 Da, globulin 165.000 Da, and fibrinogen 200.000.
Accordingly, serum globulin and fibrinogen cannot pass through, serum albumin can pass through, but the amount filtered is very small, and therefore, it would be reabsorbed back in the renal tubules; normally urine is free of plasma proteins. if the kidney becomes diseased, its permeability increases and so serum albumin will appear in the urine in large amounts. When the disease of the kidney is advanced, serum globulin will also appear in the urine. Fibrinogen will never appear.
The molecular weight of hemoglobin is 68.000 but it is normally protected by being enclosed inside the membrane of RBCs. If hemolysis occurs, hemoglobin will be set free and because of its molecular weight, will pass through the glomeruli of the kidney; this is dangerous because in the renal tubule, the reaction is acidic and so hemoglobin will be precipitated as acid hematin which blocks the renal tubules leading to anuria and death.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Suprarenal glands (adrenal glands) anatomy, structure & Effect of Deficiency of Catecholamines
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia
Juxtaglomerular apparatus structure, function & Autoregulation of glomerular filtration rate
Functions of the loop of Henle, distal tubules, collecting ducts & Glucose tubular maximum