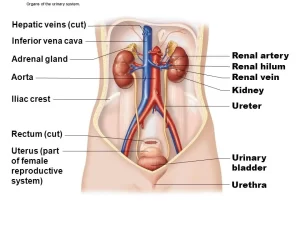
Urinary passages function, structure of Ureter, Urinary bladder and Uvulae vesicae
The urinary passage begins with the minor calyces that pour the formed urine into the major calyces. These, in turn, open into the renal pelvis, which drains into the ureters. All these passages are lined by transitional epithelium.
Ureter
- Definition: It is the muscular tube responsible for the transfer of urine collected in the kidney to the urinary bladder.
- Length: 25-30 cm (10 inches).
- Width: not more than 5mm.
- Start: superiorly, as a widened part results from joining up of the major calyces, the renal pelvis.
- End: inferiorly, by oblique pass through the lateral angle of the urinary bladder
- Renal pelvis: it is a funnel shape upper expansion of the ureter. It is dilated into 2-3 major calyces. It may lie completely outside the kidney or buried inside the substance of the renal hilum.
- Divisions: its upper half courses in the abdomen (abdominal part) while its lower half courses in the pelvis (pelvic part). So, the ureter has two divisions: the abdominal and pelvic parts.
Sites of ureteric constrictions
- Pelvi-ureteric junction.
- Point of crossing the pelvic brim or the common iliac vessels (a point halfway between the abdominal and pelvic ureter).
- Intramural part of the ureter (inside the wall of the urinary bladder).
Course and relations
1)- Abdominal part of the ureter
The ureter descends vertically on the psoas major muscle then crosses the bifurcation of the common iliac artery over the sacroiliac joints to enter the pelvis.
Right ureter
Anterior:
- Peritoneum, gonadal vessels.
- Duodenum.
- Root of mesentery.
- Terminal ileum.
- Two vessels (right colic & ileocolic).
Posterior: Psoas major, genitofemoral nerve.
Medial: Inferior vena cava.
Left ureter
Anterior:
- Two vessels (left colic & Inferior mesenteric).
- The apex of the pelvic mesocolon.
Medial: Inferior mesenteric vessels.
2) Pelvic part of the ureter
the ureter crosses the end of the common iliac artery (under the apex of the pelvic mesocolon, On the left side), it descends downwards & backwards, on the sidewall of the pelvis. The intramural part of the ureter is 1-2 cm length, oblique part inside the wall of the bladder.
Blood supply of the ureter
1) Abdominal part:
- Arterial supply: by nearby arteries; renal artery, abdominal aorta, gonadal and common iliac.
- Venous drainage: through renal vein, gonadal and internal iliac veins.
2) Pelvic part:
- Arterial supply: by inferior vesical (in males) or uterine & vaginal arteries (in females).
- Venous drainage: through venae comitants of the supplying arteries which drain into the internal iliac veins.
Lymphatic drainage: to the para-aortic lymph nodes.
Histological structure of the wall of the ureter
In cross-section, the ureter in the empty state has a stellate-shaped, narrow lumen. It is formed of the following layers.
Mucosa
- The surface epithelium: lined by the transitional epithelium “urothelium” resting on a thin corrugated basement membrane.
- The lamina propria: loose connective tissue rich in elastic fibers.
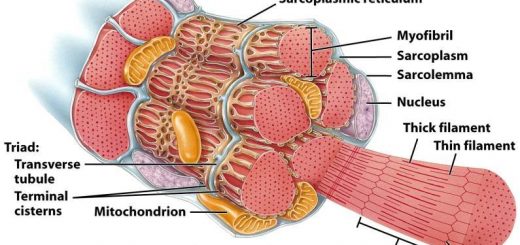
Musculosa
- It is responsible for the slow peristaltic contractions forcing urine in unidirectional pulses down into the bladder.
- The smooth muscle fibers are arranged as: Inner longitudinal and outer circular layers. At the lower third of the ureter, an outer longitudinal layer is added.
- Bundles of muscle fibers are separated by abundant elastic connective tissue to allow distention of the wall when filled by urine.
Adventitia: It is formed of fibro-elastic connective tissue that binds the ureter to the surrounding structures.
Urinary bladder
It is a hollow muscular organ acting as a reservoir for urine.
Site
- It is a hollow muscular organ acting as a reservoir for urine.
- In infants & children up to 3 years: it is an abdominal organ (due to narrow pelvis).
- In children above 3 years up to adult age: the bladder starts to enter the pelvic cavity.
- In adults: it is a pelvic organ.
Shape
- Empty bladder; it has a shape of three-sided pyramid.
- It has 4 surfaces; superior, two inferolateral & posterior (base).
- 4 angles: anterior (apex), inferior (neck), and two posterosuperior.
- 3 attached tubular structures; two ureters & urethra.
- 4 ligaments; median umbilical ligament, pubovesical or puboprostatic, and 2 lateral ligaments of the urinary bladder.
Surfaces and relations: Each surface is triangular in shape.
Superior surface
It is covered by the peritoneum and related to the superior vesical artery and coils of the ileum. Other relations differ between males and females.
- Males: Rectovesical pouch of the peritoneum, pelvic colon.
- females: uterovesical pouch of the peritoneum, the anterior wall of the fundus, and body of the uterus.
Inferolateral surface
It is related to:
Anteriorly:
- Pubic bone.
- Retropubic space [fat + ligament pubovesical (female) or puboprostatic (male)].
Posteriorly:
- Obturator internus muscle.
- Obturator vessels and nerves.
- Levator ani muscle.
Posterior surface (base of the bladder):
Male:
- Rectum.
- Two ampullae of vas deferens.
- Two seminal vesicles.
- Rectovesical pouches of the peritoneum (to the uppermost part of the base).
Female:
- Vagina.
- Anterior vaginal fornix.
- Cervix.
Position:
Inside the pelvic cavity, it is situated with its:
- apex, facing anteriorly, related to the upper border of the symphysis pubis.
- base, facing posteriorly.
Angles of the urinary bladder
Anterior angle (apex): it is attached to the umbilicus by a median umbilical ligament (obliterated urachus which is a tubular structure present during the development of the bladder and becomes fibrosed in adult age). The other end of the median umbilical ligament is attached to the umbilicus.
Inferior angle (neck): It is the point of meeting the base with the two inferolateral surfaces of the bladder. It lies 1 inch behind the lower border of the symphysis pubis. The urethra gets an exit from this point. It is surrounded by the base of the prostate in males and pelvic fascia in females.
Two posterosuperior angles: The two ureters enter the bladder at these angles.
Ligaments of the bladder
To the apex: median umbilical ligament.
To the neck: pubovesical (female) or puboprostatic (male).
- Pubovesical ligament: it is attached anteriorly to the posterior surface of the body of the pubic bone near the midline and to the neck of the bladder and upper part of the urethra posteriorly.
- Puboprostatic ligament: it is attached anteriorly to the posterior surface of the body of the pubic bone near the midline and to the neck of the bladder and the base of the prostate, posteriorly.
To the posterosuperior angles: lateral ligament of the urinary bladder. It is a dense pelvic fascia, extending from the lateral pelvic wall to the two posterosuperior angles.
Interior of the bladder
- In an empty bladder, the mucosa is thick and has folds (rugae).
- In full bladder, it is thin and smooth.
Trigone
It is a triangular area, that can be seen in the mucosa of the posterior wall of the bladder, between three openings; two ureters and internal urethral meatus. It has a smooth surface even in an empty bladder, due to its embryonic origin (mesodermal not endodermal like the other mucosa). It is more vascular, sensitive, and elastic than the other mucosa. It contains a special smooth muscle called superficial trigonal muscle that:
- May help in closure of the ureteric orifice during bladder contraction.
- Extends to the proximal part of the urethra in both sexes.
Factors preventing urine reflux to the ureter during bladder contraction
- Very oblique course of the intramural part of the ureter.
- A valve-like flap of mucosa at the ureteric orifice.
Interureteric bar: It is raised transverse ridge between the two ureteric orifices.
Uvulae vesicae
It is a small rounded elevation that lies immediately behind the internal urethral opening. It is caused by the protrusion of underlying middle lobe of the prostate.
Blood supply of urinary bladder
Arterial supply: by the following arteries:
- Superior vesical, for the superior surface.
- Inferior vesical (in males) or vaginal (in females), for the base and trigone.
- Middle rectal (in males).
- Obturator
- Inferior gluteal.
Venous drainage: through the vesical venous plexus (surrounding the bladder) which drains into the vesico-prostatic venous plexus (surrounding the vesico-prostatic groove) which drains into the internal iliac vein.
Lymphatic drainage: Lymphatic vessels travel with the blood vessels to reach the internal iliac lymph nodes and then to the para-aortic lymph nodes.
Urinary bladder pain is carried by afferent pain nerve fibers, which ascends with the sympathetic system. So the referred pain is felt in the dermatome of L1,2 (pubic region, groin, anterior external genital area, and front of the thigh).
Nerve supply
The urinary bladder consists of a main portion (body) that collects urine and a funnel-shaped extension (neck) that connects with the urethra. Three poorly defined layers of smooth muscle make up the bulk of the bladder wall, the so-called detrusor muscle.
The wall of the posterior urethra contains smooth muscle fibers of the detrusor muscle interspersed with elastic tissue, together forming the internal sphincter. Immediately adjacent is the external sphincter, made up of voluntary, striated-muscle fibers. The bladder and sphincters receive sympathetic and parasympathetic (autonomic) as well as somatic (voluntary) innervation.
1) parasympathetic fibers
The pelvic nerves are mainly connected with S2,3 and S4 segments. Coursing through the pelvic splanchnic nerves are both sensory and motor fibers. The sensory fibers detect the degree of stretch of the bladder wall. The motor fibers are parasympathetic fibers that terminate on ganglion cells located in the wall of the bladder. Short post-ganglionic nerves then innervate the detrusor muscle. The parasympathetic activity contracts the detrusor muscle and relaxes the trigone and internal sphincter. Thus, the pelvic nerves are the main nerves of micturition.
2) Sympathetic fibers
Sympathetic innervation, from the sympathetic chain through the hypogastric nerves, is connected mainly with the L1-2 segment of the spinal cord. They cause vaso constriction of blood vessels of the urinary bladder, as well as relaxation of detrusor muscle and contraction of the internal sphincter resulting in urine retention. Some sensory nerve fibers also pass by way of the sympathetic nerves and may be important for the sensation of fullness and perhaps pain in some instances.
Urinary bladder pain is carried by afferent pain nerve fibers, which ascends with the sympathetic system. So the referred pain is felt in the dermatome of L1,2 (pubic region, groin, anterior external genital area, and anterior thigh).
3) The pudendal nerve
It supplies the external sphincter of the bladder. These somatic nerve fibers innervate the skeletal muscle of this sphincter.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition
Control of water balance in your body, Regulation of volume & osmolality of Body fluids
Osmolality, Concentrating mechanism of the kidney, Urine concentration & dilution
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism