Urinary incontinence treatment, types, causes and How to stop urine leakage
Urinary incontinence is the involuntary leakage of urine, which can vary in severity from occasional dribbles to full loss of bladder control. It affects people of all ages and genders, although it is more common in older adults, particularly women.
Types of urinary incontinence
- Stress Incontinence: Occurs when physical movement or activity (e.g., coughing, sneezing, laughing, or exercising) puts pressure on the bladder, causing urine to leak.
- Urge Incontinence is characterized by a sudden, intense urge to urinate, followed by an involuntary loss of urine, This may be associated with an overactive bladder, and conditions such as urinary tract infections, neurologic disorders, or diabetes.
- Overflow Incontinence takes place when the bladder doesn’t empty completely, leading to dribbling. It’s often caused by a blockage or an underactive bladder muscle.
- Functional Incontinence: A result of physical or mental impairments that prevent a person from reaching the toilet in time, even though the urinary system is functioning normally (e.g., due to arthritis or dementia).
- Mixed Incontinence: A combination of two or more types of incontinence, usually stress and urge incontinence.
Causes of Urinary incontinence
- Weak pelvic floor muscles (common after childbirth or with aging).
- Bladder or prostate problems.
- Neurological conditions (e.g., stroke, multiple sclerosis).
- Certain medications.
- Hormonal changes during menopause.
- Obesity.
Treatment options
- Lifestyle changes: Managing fluid intake, avoiding bladder irritants (like caffeine), weight loss, and bladder training.
- Pelvic floor exercises: Kegel exercises strengthen the muscles that control urination.
- Medications: Drugs may help relax the bladder or tighten the sphincter.
- Medical devices: Pessaries or urethral inserts can help in certain cases.
- Surgical options: These might be considered for severe cases, such as sling procedures for stress incontinence.
- Behavioral therapies: Timed voiding or bladder retraining.
- Managing urinary incontinence typically involves a combination of these treatments, tailored to the type and severity of the condition.
Lines of treatment
1. Non-pharmacologic Treatment
Behavioral therapies require functional capacity, learning ability, and patient motivation, Lifestyle and behavioral interventions are the first-line treatment of choice in the elderly population, Lifestyle modifications include smoking cessation, caffeine and alcohol reduction, weight loss, and modified fluid intake.
Bladder training is an urge suppression technique, The patient gradually increases toileting intervals by resisting or inhibiting the sensation of urgency. Patients learn to urinate according to a scheduled timetable.
Distraction and relaxation techniques are employed to help delay voiding and allow the development of increased bladder capacity, The interval is initially based on the patient’s voiding habits and increased by 15-to 30-minute increments per week until a voiding interval of 3-4 hours is achieved. Regular voiding at timed intervals avoids a full bladder or prevents involuntary bladder contractions.
Pelvic muscle rehabilitation (Kegel exercises), Repetitive contraction, and relaxation of the pelvic floor muscles are used to improve the reflex inhibition of involuntary detrusor contractions and enhance the ability to contract the external sphincter voluntarily.
Sacral nerve stimulation (SNS) has FDA approval for use in the treatment of patients with severe refractory UI when behavioral management and medications fail or are not tolerated. In SNS, a generator device is inserted subcutaneously in the lower back or buttocks, A lead is attached to the $3 sacral nerve, and electrical stimulation results in decreased contraction of the detrusor muscle.
Women with good manual dexterity are candidátes for intravaginal support devices or urethral occlusion inserts, Pessaries are often employed in older women who have not responded to behavioral therapies.
Urinary catheters are reserved for patients with chronic bladder-emptying difficulty and elevated PVR, Severely or terminally ill patients with chronic UI who are bedridden.
2. Invasive treatment
- Surgery is the most effective treatment for SUI.
- Periurethral injection of bulking agents (e.g., collagen) improves urethral closure in SUI.
- Although not a first-line therapy) artificial urinary sphincters are the most effective treatment for intractable post-prostatectomy SUI in men (complications: infections, tissue atrophy resulting in worsening incontinence, urethral erosion, and device defects).
3. Pharmacological therapy
Pharmacotherapy does not cure UI. It is often added to behavioral therapy to help alleviate symptoms. Antimuscarinics: The most commonly prescribed UI drug, Oxybutynin remains the gold standard and the first approved antimuscarinic agent for UI. extended-release formulation is preferred due to less anti-cholinergic side effects. new drugs: Solifenacin 5 &10mg, Darifenacin 7.5 &15 mg.
Duloxetine: The 2012 European Association of Urology Guidelines recommends duloxetine to both men and women with SUI (grade A evidence level). In the 2012 American Geriatrics Society Beers Criteria, duloxetine was listed for use with caution in elderly patients because of the risk of syndrome of inappropriate antidiuretic hormone or hyponatremia. Duloxetine is not recommended when the CrCl is less than 30 mL/minute.
α-agonists are not as common now that duloxetine is considered a first-line agent. Some guidelines do not even list α-agonists as an option for treatment anymore.
Estrogens: Oral and topical estrogen therapy was thought to improve the symptoms of SUI by increasing α-receptors and local circulation. Both the Heart and Estrogen/Progestin Replacement Study (HERS) and the Women’s Health Initiative study showed worsening UD with the use of oral estrogen.
The 2012 European Association of Urology guidelines endorse topical estrogen as an option for SUI (grade A level. recommendation). The 2012 Beers Criteria recommends against the use of oral or transdermal patch estrogen in women.
Botulinum Toxin: In 2011, the FDA approved onabotulinum toxin A for use in patients with detrusor overactivity associated with a neurologic condition (e.g., spinal cord injury, multiple sclerosis) and inadequate response to anticholinergic therapy.
Mirabegron: a new β3-adrenergic receptor agonist, was approved in mid-2012 for the treatment of OAB with urgency symptoms. Stimulation of the β3-receptor causes bladder relaxation during filling.
Treatment for each type of urinary incontinence
1. Detrusor overactivity: (Urge incontinence)
Behavioral therapy: patients must void every 1-2 hours while awake; when continence is restored, the intervals is increased by 30 minutes until it reaches 4-5 hours, most of continent patients at the day are also continent at night. If this is impossible patient should be asked if they need to void at suitable intervals.
Pelvic floor exercises: can be added to behavioral approaches; helps train patient with intact cognitive functions and well-motivated. If the above is insufficient, drug therapy to relax the Detrusor muscle should be attempted.
Drugs: (Antimuscarinics): Oxybutinin 2.5-5 mg 3 or 4 times daily, long-acting Oxybutinin 5-15 mg daily, and Tolterodine 1-2 mg twice daily may reduce episodes of incontinence.
Sacral nerve stimulators in severe UUI: In refractory cases, if intermittent catheterization is possible, the physician may intend to induce urine retention with bladder relaxant and then empty the bladder 3-4 times daily. If all measures fail, an external collection device or protective pad or undergarment may be required.
2. Stress incontinence
Surgery is the last method but it is the most effective treatment leading to a cure of 75-85% even in older women. Pessary may provide some relief for women with vaginal stenosis.
Pelvic floor exercise can be done by asking the patient to contract the muscle that is used to stop the flow of urine 30-60 exercises daily for 6 weeks is performed before significant improvement is noticed. In mild to moderate cases, it is effective; it can be combined with electrical stimulation or vaginal cones.
Drugs:
- Duloxetine (may be used first line).
- Antimuscarinics.
- Topical or oral estrogen is of low effect unless atrophic vaginitis with urethral irritation is present.
- α-Agonists (third line).
3. Urethral obstruction
- Surgical decompression is the most effective treatment, especially if it is associated with retention of urine.
- For the non-operative candidate with urinary retention intermittent or indwelling catheterization is used.
- In men with prostatic obstruction without retention and who refuse surgery. He must be treated with: α-blocking agent: e.g. trazosin 1-10 mg daily, Prazosin 1-5 mg orally twice daily or tamsulosin 0.4-0.8 mg daily may relieve symptoms. 5-α reductase inhibitors (finasteride).
4. Detrusor under activity: (Overflow incontinence)
- If the bladder is poorly contractile, augmented voiding techniques such as double voiding, and suprapubic pressure often prove effective.
- If a patient needs further emptying, an intermittent or indwelling catheter is the only option.
- Antibiotics should be used only for symptomatic infection or as prophylaxis against recurrent symptomatic infection, i.e. in patients using intermittent catheterization. But not used as prophylaxis with an indwelling catheter.
5. Functional incontinence
Implement lifestyle interventions.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Urinary incontinence in elderly causes and treatment, How to correct urinary incontinence?
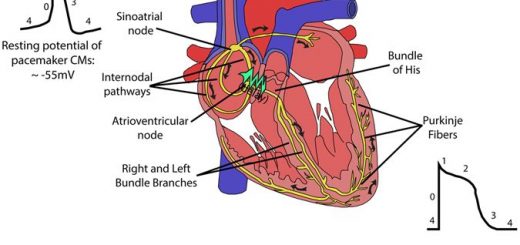
Properties of cardiac muscles, Cardiac automaticity, and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure, and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk, and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart and Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function