Urinary bladder structure, function, Control of micturition by Brain and Voluntary micturition
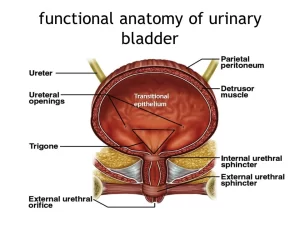
The urinary bladder is located in the pelvic cavity, posterior to the symphysis pubis, and below the parietal peritoneum, It is a hollow muscular organ in humans and other vertebrates, It stores urine from the kidneys before disposal by urination, The size of the urinary bladder varies with the amount of urine it contains and with the pressure it receives from surrounding organs.
Histological structure of the wall of the urinary bladder
The urinary bladder or simply bladder is a hollow distensible organ that sits on the pelvic floor, In cross-section, it has a relatively wide lumen and thick wall, It is formed of the following layers:
Mucosa
It shows numerous folds that disappear when the bladder becomes distended with urine, except the mucosa of the trigone which is always smooth and not folded.
- The surface epithelium: the urothelium resting on the thin corrugated basement membrane.
- The lamina propria: vascular connective tissue rich in elastic fibers.
Adaptation of the transitional epithelium (urothelium) to function
The transitional epithelium particularly its superficial dome-shaped cells (umbrella cells), displays unique features that allow volume change in the urinary passages and form an osmotic barrier. These features are most prominent in the urinary bladder where contact with urine is greatest. These include:
- The luminal membrane of dome-shaped cells is thickened by membranous plaques connected by inter plaque regions.
- The apical cytoplasm contains fusiform vesicles formed by membranes identical to that of the plaques.
- Bundles of intermediate filaments and microfilaments are stretching from the inner surface of the plaques into the vesicles.
- Occluding junctions are present between the adjacent dome-shaped cells.
A. Volume change in the bladder
When the bladder is distended:
- The epithelium becomes thinner (about 2-3 cells thick) with flattened cells.
- The filaments in the superficial dome-shaped cells pull the fusiform vesicles to become inserted as plaques into the luminal surface, thus increasing the bladder surface area.
When the bladder is empty:
- The epithelium regains its full thickness (6 layers or more).
- The filaments in the superficial dome-shaped cells pull the plaques to become detached from the luminal surface and are internalized as fusiform vesicles, thus decreasing the bladder surface area.
B. Osmotic barrier (Urinary bladder barrier)
It consists of:
- The thickened luminal membrane of the superficial dome-shaped cells impermeable plaques.
- The intercellular occluding junctions between these cells.
This barrier serves to:
- Protect the bladder epithelium from toxic wastes present in urine.
- Prevent leakage of urine into the extracellular spaces.
- Prevent dilution of the hyperosmotic urine by the capillaries in the lamina propria
Musculosa
The smooth muscle fibers are arranged as; inner and outer longitudinal layers and a middle circular layer, collectively known as detrusor muscle. The muscle fibers are in the form of bundles separated by abundant fibro-elastic connective tissue to allow bladder distension, At the neck of the bladder, dense bundles of circular smooth muscles surround the urethra forming the internal urethral sphincter.
Adventitia
It is formed of fibro-elastic connective tissue. The superior surface of the bladder is covered by the visceral peritoneum i.e. SEROSA.
Urethra
It is a muscular tube that conducts the urine from the (urinary bladder) and semen from the (ductus deferens) to the exterior, It starts at the neck of the urinary bladder, as the internal urethral opening, and ends externally in the urogenital triangle of the perineum, as the external urethral opening.
Male Urethra
- The male urethra is S-shaped duct about 20 cm (or 8 inches) in length.
- It begins at the neck of the bladder then extends through the prostate, pelvic diaphragm, sphincter urethrae, root & body of the penis to end at the tip of the glans penis as an external urethral orifice.
- It serves as the terminal passage for both the urinary and reproductive systems.
Course & Relations
1. Prostatic part
It is 3 cm (1.5 inch) long and fusiform in shape. It extends from the internal urethral orifice at the apex of the trigone of the bladder → traverses the prostate → ends at the external urethral sphincter muscle, Its proximal part is surrounded by the internal urethral sphincter which helps to close this opening during the ejaculation to prevent the regurgitation of the seminal fluid, It is the widest & most dilatable part of the urethra, It is lined by transitional epithelium, It contains the openings of the ejaculatory ducts and the small ducts draining the sperms.
2. Membranous part
1 cm (0.5 inch) long. It starts at the apex of the prostate, passes through the pelvic diaphragm and sphincter urethrae (deep perineal pouch) to end at the bulb of the penis. It is the shortest, narrowest & least dilatable part of the urethra, It lies in the deep perineal pouch and is surrounded by the external urethral sphincter, Its wall is thin so it is most liable to rupture during instrumentation (catheter), and it is lined by pseudostratified columnar epithelium.
3. Spongy part (Penile urethra)
10 to 16 cm (6 inches) long. It extends from bulbs to the body to glans of penis ending at the external urethral orifice (longest & narrowest part of the male urethra), It lies in the corpus spongiosum of the penis, It shows 2 dilatations; in the bulb (intrabulbar fossa) and in the glans (fossa navicularis).
It is lined by pseudostratified columnar epithelium with areas of stratified columnar. In the glans penis, it is lined by non-keratinized stratified squamous epithelium. It contains the openings of ducts of the mucus-secreting bulbourethral glands (Cowper’s glands) and the urethral glands of Littré.
Female Urethra
The female urethra is about 4 cm, long extending from the internal to the external urethral orifices, It is wider and more dilatable than the male urethra, It begins from the bladder neck at the internal urethral orifice, and descends downwards and forwards, traversing the deep and superficial perineal pouches.
It ends by the external urethral orifice into the vestibule of the vagina between the clitoris and the vaginal opening. Its upper (initial) part: is surrounded by the sphincter urethrae, It is connected to the inferior part of the pubic bone by the pubovesical ligament. It is:
- Anteriorly: separated from symphysis pubis by fat.
- Posteriorly: adherent to the anterior wall of the vagina.
It is exclusively a passage for urine lined by transitional epithelium at the initial part then stratified squamous epithelium. The lamina propria of the female urethra is highly vascular, It contains the openings of ducts of the mucus-secreting urethral glands of Littré.
Micturition
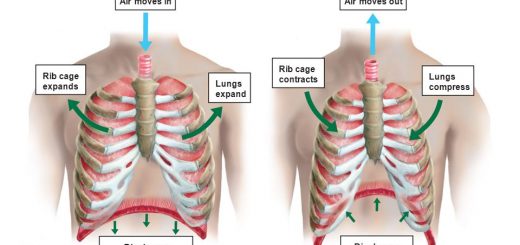
The Bladder filling (Storage phase)
Bladder tone is defined by the relationship between bladder volume and internal (intravesical) pressure (cystometrogram). Increasing bladder volume from 0 to ∼ 50 mL produces a moderately steep increase in pressure, Additional volume increases up to ∼ 300mL produce almost no pressure increase; this high compliance reflects relaxation of bladder smooth muscle which is mediated by tonic sympathetic discharge.
At volumes higher than 400 mL, additional increases in volume produce steep rises in “passive” pressure, up to the point of triggering the micturition reflex, The detrusor muscle is tonically inhibited during filling of the bladder, and such inhibition prevents urine from being voided.
Sensations of the urinary bladder
- The first desire for micturition is felt at a bladder volume of about 150 ml, and it can easily be voluntarily inhibited.
- The sense of bladder fullness (that normally initiates the micturition reflex) is felt at a volume of 400 ml, and it can also be voluntarily inhibited.
- A sense of bladder discomfort is felt at volumes between 400-600 ml, but the micturition reflex can still be voluntarily inhibited.
- A sense of bladder pain is felt at volumes exceeding 600 ml, and it can hardly be inhibited.
- When the volume reaches 700 ml, urination becomes urgent and obligatory micturition occurs.
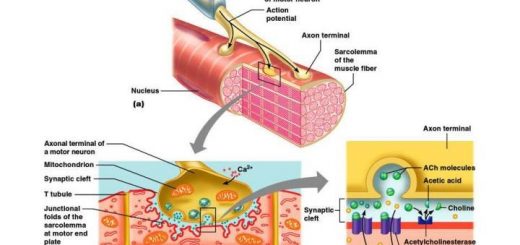
The micturition reflex
The micturition reflex is a stretch reflex, initiated by sensory stretch receptors in the bladder wall, especially by the receptors in the bladder neck when this area begins to fill with urine at the higher bladder pressures, Sensory signals from the bladder stretch receptors are conducted to the sacral segments of the cord through the pelvic nerves and then reflexively back again to the bladder through the parasympathetic nerve fibers.
Once a micturition reflex begins, it is “self-regenerative, That is, the initial contraction of the bladder activates the stretch receptors to cause a greater increase in sensory impulses to the bladder and bladder neck, which causes a further increase in reflex contraction of the bladder; thus, the cycle is repeated again and again until the bladder has reached a strong degree of contraction, The fluid pressure in the bladder becomes great enough to force the bladder neck to open despite of its tonic contraction.
Stretch of the neck not only increases the intensity of the micturition reflex itself but causes still another reflex as well, This reflex passes to the sacral portion of the spinal cord and then back through the pudendal nerve to the external sphincter to inhibit it, If this inhibition is more potent than the voluntary constrictor signals from the brain, then urination will occur, If not, urination still will not occur until the bladder fills still more and the micturition reflex becomes more powerful.
After a few seconds to more than a minute, the self-regenerative reflex begins to fatigue and the regenerative cycle of the micturition reflex ceases, permitting the bladder to relax, Once a micturition reflex has occurred and has not succeeded in emptying the bladder, the nervous elements of this reflex usually remain in an inhibited state for at least a few minutes to an hour or more before another micturition reflex occurs.
Control of micturition by the brain
The micturition reflex is a completely automatic and cord reflex, but it can be inhibited or facilitated by centers in the brain. These include:
- Strong facilitatory and inhibitory centers in the brain stem, probably in the pons.
- Several centers in the cerebral cortex which are mainly inhibitory.
Voluntary micturition
Voluntary micturition is usually initiated in the following way: First, the person contracts his abdominal muscles, which increases the pressure of urine in the bladder. At the same time, the pelvic floor muscles are relaxed, which lengthens the bladder neck and allows extra urine to enter the neck under pressure, thus stretching its walls, This then excites the stretch receptors, which excites the micturition reflex, and at the same time inhibits the external bladder sphincter, Ordinarily, all the urine will be emptied with rarely more than 5 to 10 milliliters left in the bladder.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Urinary passages function, structure of Ureter, Urinary bladder & Uvulae vesicae
Control of water balance in your body, Regulation of volume & osmolality of Body fluids
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Physical properties of urine, Tests to evaluate kidney function & Normal constituents of urine