Upper GI bleeding, Acute Erosive Gastritis causes and risk factors, How do you treat erosive gastritis?
Acute erosive gastritis is a sudden inflammation of the stomach lining characterized by superficial erosions (small breaks in the mucosa) caused by irritants like medications, alcohol, or infections. Unlike chronic gastritis, this condition develops quickly and can lead to significant stomach discomfort or bleeding.
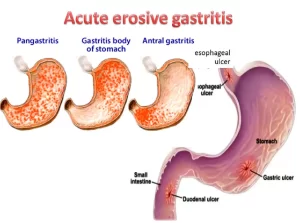
Acute Erosive Gastritis
Diffuse superficial mucosal lesions in the body and fundus may duodenum.
Causes
- NSAID.
- Alcohol.
- Drugs.
- Long-distance running.
- Gastric irradiation.
- 50% mortality with surgery.
NSAID-induced ulcer
The risk of bleeding is increased with:
- Increasing dose (dose-related).
- When two or more are taken together.
- Concomitant anticoagulant or corticosteroid.
Options:
- Near total gastrotomy + Roux en Y.
- Ligation of all blood vessels to the stomach.
- Vagotomy & pyloroplasty.
- Conserve until transfusion requirement is 12 units or more.
Causes & Risk Factors
Medications:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) like aspirin, ibuprofen, and naproxen.
- Corticosteroids.
Alcohol & Smoking:
- Excessive alcohol consumption damages the stomach lining.
- Smoking increases acid production and weakens mucosal protection.
Infections:
- Helicobacter pylori (H. pylori) infection.
- Viral or bacterial infections (especially in critically ill patients).
Stress-related Gastritis:
- Severe burns (Curling’s ulcer), trauma, surgery, or shock.
- Critically ill patients (ICU patients with ventilators or sepsis).
Chemical & Toxin Exposure:
- Ingestion of corrosive substances (acids, alkalis).
- Chemotherapy and radiation therapy.
Symptoms
- Upper abdominal pain (burning, gnawing).
- Nausea and vomiting (may contain blood in severe cases).
- Loss of appetite.
- Black, tarry stools (melena) – A sign of gastrointestinal bleeding.
- Vomiting blood (hematemesis).
Complications
- Gastrointestinal bleeding – Can cause anemia, weakness, and shock in severe cases.
- Ulcer formation – Erosions may develop into peptic ulcers.
- Perforation (rare but serious) – A hole in the stomach wall leading to peritonitis.
Diagnosis
- Endoscopy (EGD – Esophagogastroduodenoscopy) – Gold standard for detecting erosions, inflammation, or bleeding.
- H. pylori Testing – Blood, stool, breath test, or biopsy.
- Blood Tests – To check for anemia (low hemoglobin).
- Stool Test (Occult Blood Test) – Detects hidden blood in the stool.
Treatment
Medications:
- Proton Pump Inhibitors (PPIs) – Omeprazole, pantoprazole, esomeprazole (reduce stomach acid).
- H2 Receptor Blockers – Ranitidine, famotidine (less commonly used now).
- Antacids – Neutralize stomach acid and relieve symptoms.
- Cytoprotective Agents – Sucralfate (coats stomach lining), Misoprostol (protects against NSAID damage).
- Antibiotics – If H. pylori is detected.
Lifestyle Changes:
- Avoid NSAIDs, alcohol, and smoking.
- Eat a bland diet (avoid spicy, acidic, and fried foods).
- Manage stress with relaxation techniques.
Treatment of Underlying Conditions:
- ICU patients may receive prophylactic PPIs to prevent stress ulcers.
- If severe bleeding occurs, endoscopic intervention (cauterization or clipping of bleeding vessels) may be needed.
Prevention
- Use NSAIDs cautiously – Take with food and only when necessary.
- Limit alcohol intake.
- Treat H. pylori infections early.
- Maintain a healthy diet and avoid irritants.
Mallory Weis tear
- 13-14% of upper GI bleeding, Transient increase in P. gradient between the intrathoracic and intragastric portion of GOJ.
- 50% protracted nausea and vomiting followed by haematemsis,
- Diagnosis should not be restricted to patients with an antecedent history of N & V.
- Linear, longitudinal fissure-like tear at or below the GOJ.
- Tears are usually found on the lesser curve.
- 30% single, 19% two, 7% three, length >2 cm. Endoscopy: active spurter, oozing, clot or spot.
- Patient with MW with portal hypertension →diffuse venous bleeding and tendency to continued bleeding 90%.
Patient:
- with bleeding →endoscopic intervention.
- no bleeding→ No intervention.
- Rebleeding in 0.2%.
Dieulafoy’s lesion
- 0.5-5.3% of upper GI bleeding.
- Caliber-persistent artery that fails to narrow in size as they penetrate the submucosa (histology normal artery).
- Most common within 6 cm of the GOJ in the fundus.
- Nipple or volcano with a central whitish discoloration with no ulcerated base in the fundus (not ulcer with the visible vessel).
- Recurrent massive haematemsis without prodromal symptoms.
- Treatment: Endoscopic or surgical.
Upper GI bleeding notes
Massive bleeding from varices or duodenal ulcers for example may result in fresh rectal bleeding (bright blood). IF NG aspirates are positive (containing blood), the patient is admitted to the unit, after using the treatment methods, banding for example, the patient can morally eat if the aspirate is green or yellow (bile).
In causes of OV, varices, oesophagitis, ulcers, and neoplasms are the most common. In causes of stomach bleeding, gastritis, gastric cancer, gastric ulcers, and gastric varices are the most common. In causes of the duodenal bleeding, erosive duodenitis and duodenal ulcers are the most common.
There is a decrease in the incidence of peptic ulcers but not complicated duodenal ulcers although causes are still persisting; hyperacidity, and a decrease in mucosal resistance. We should note that there is incidence of bleeding without symptoms (chronic asymptomatic ulceration).
Posterior ulcers are more severe and result in severe torrential bleeding. Rebleeding is a bad prognostic sign and increases the mortality to 10 fold. OV rebleed within 5 days while non-esophageal varices rebleed within 2-3 days. Now drugs are given in large doses and rapidly to exert an appreciable effect on the outcome of the bleeding.
Avoid blood transfusions if there is no significant need to avoid: heart failure, pulmonary edema, and bleeding recurrence. A laser photocoagulation device is not suitable for patients who are Haemo dynamicaly unstable as we should move the patient to the laser not the laser to the patient.
Injection treatment of ulcers has triple action; mechanical compression, platelet activation, and vasospasm. TAE is a transcatheter arterial embolism, injection of chemotherapeutic agents such as gelatin foam, coils, or both or histoacryl through the femoral artery then selectively to the bleeder.
From the indications of the surgery; failure of the endoscopic trials and massive spurter post ulcer bleeding. For surgery lines, now vagotomy is better than gastrectomy due to its high mortality. The common causes of acute erosive gastritis are: NSAID (of all types), alcohol and drugs.
In acute erosive gastritis, conservation (medical treatment without surgery) is required until transfusion requirements are 12 units or more as surgery carries a high risk of mortality 50% which is not acceptable). In variceal bleeding conservative treatment, avoid saline due to sodium and water retention, in non-variceal. it is acceptable to introduce saline.
In general plan of treatment to guard against liver failure and encephalopathy; an NG tube is applied to remove blood from the stomach, rectal wash is applied to remove blood from the lower portion, introduce intestinal antiseptic and hypertonic glucose slowly.
Glypressin is now used instead of vasopressin. In injection treatment for bleeding OV, we inject ethanolamine oleate sodium morrhuate and polidocanol while in bleeding GV we use histoacryl.
In bleeding varices, if conservation, endoscopic or banding ligations fail, surgery is the choice and mainly oesophageal transaction; it is easy but it is liable for recurrence, and multiple sessions of band ligation or injection are required. Note that emergency decongestion is liable for 50% recurrence and 40% portal vein thrombosis, portocaval has high mortality and is irreducible. Banding is better than sclerotherapy.
You can subscribe to Science Online on YouTube from this link: Science Online
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
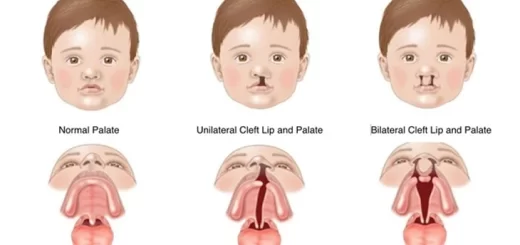
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion