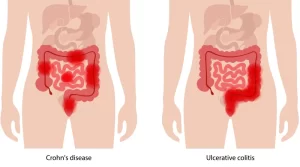
Ulcerative colitis causes, symptoms, treatment and can ulcerative colitis be cured?
Ulcerative Colitis causes inflammation and ulcers (sores) in the lining of the colon. It is a chronic inflammatory bowel disease (IBD) that affects the large intestine (colon), This inflammation can lead to a variety of symptoms, including Diarrhea, Rectal bleeding, Abdominal pain and cramping, Urgent need to have a bowel movement, Fatigue, and Weight loss.
Ulcerative colitis
Sudden acute diarrhea (blood + mucus) not responding to usual treatment, we have to exclude infectious diarrhea, definite diagnosis is by colonoscopy and biopsy.
Symptoms of Ulcerative colitis
Symptoms can vary in severity and may include:
- Persistent diarrhea.
- Rectal bleeding.
- Abdominal pain and cramping.
- Urgent need to have a bowel movement.
- Weight loss.
- Fatigue.
- Loss of appetite.
Site
- Limited to Large intestine.
- Rectosigmoid in 30% (Proctitis).
- Up to hepatic flexure (Distal UC).
- Proximal to hepatic flexure (extensive UC). if the entire colon = Pancolitis, if pancolitis with terminal ileum = ileal backflush. The rectum is involved in 95%, while the anal canal is almost always spared.
Pathology
Gross Pathology
- Erythema, edema.
- Begins in the rectum and ascends.
- The sharp line of demarcation between healthy and unhealthy.
- Inflammatory polyps or pseudo-polyps.
- Loss of haustration, flat appearance.
- In extremely ill toxic megacolon (Colonoscopy is contraindicated & Barium enema is also contraindicated).
MP
Crypt abscess neutrophils in lamina propria, the inflammatory process does not disrupt muscularis mucosa. Variable degree of atrophy and dysplasia.
Clinical picture:
- Dysentery Rectum is almost always involved.
- Extent: May be: Pancolitis 30%. 30-40% is limited to Rectosigmoid. 30% It sided colitis. The rest is intermediate.
- Fever, tenderness, anemia, albumin decrease.
- Some patients complain of diarrhea alone or blood/rectum alone.
- 15-25% extraintestinal manifestation (EIM).
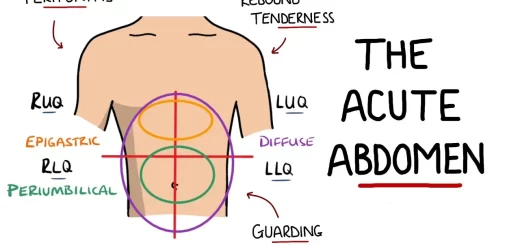
Intestinal complications
- Patients with toxic megacolon present with fever, tachycardia 120/min, abdominal distension, localized peritonitis, dilated colon on plain X-ray, leucocytic count > 11,000, no Barium enema, no colonoscopy.
- Perforation: Severe colitis → Perforation (mostly in sigmoid colon) high mortality rate.
- Stricture: It is uncommon, if present suspect malignancy. Massive hemorrhage: If uncontrollable treatment is by colectomy.
- Cancer is related positively to the duration and the extent of the colon involvement colonoscopy every year, if dysplasia is present → total colectomy.
Diagnosis
Diagnosis depends on clinical, radiologic endoscopic, and histologic finding. ANCA is not diagnostic alone but confirms other criteria.
I. Laboratory findings
- Leukocytosis.
- Thrombocytosis.
- – Anemia: (Fe decreases anemia of chronic disease and blood loss).
- ESR & CRP increase.
- Stool analysis leucocytes.
- Serology: PNACA: 60% UC. ASCA +ve: 60% CD.
- Specific stool test: Fecal Calprotectin. Fecal Lactoferrin.
II. Imaging studies
- Barium enema is inferior to colonoscopy to evaluate the extent of mucosal involvement in the colon. Reflux of barium into the terminal ileum may provide documentation of ileal disease which differentiates Crohn’s disease from UC.
- Plain x-ray for: Intestinal obstruction, and Toxic megacolon.
IIL Endoscopy
Colonoscopy:
- The procedure of choice for evaluating the presence and extent of UC. It also allows for intubation of the terminal ileum.
- Biopsy is taken from normal and diseased areas.
- Superficial continuous ulceration with rectal involvement.
Differential Diagnosis
- UC versus CD: Indeterminant colitis.
- IBS.
- Infectious colitis.
- Conditions mimic IBD (e.g. Diverculitis, Appendicitis, Lymphoma, Malignancy).
- Non-infectious colitis.
Treatment of UC
I. Sulfasalazine
Sulfasalazine remains the drug of choice 2-4 grams, we use it alone with local treatment in mild and moderate diseases mild < 4 motions/day in moderate we use also 5 ASA enema and suppository and hydrocortisone enema, 2 weeks before accepting the failure of treatment. Moderate disease 4-6 motions/day.
II. Corticosteroids
- If no response we start oral cortisone 40-60mg for 3-4 weeks to attain remission then start withdrawal fluids.
- JV withy prednisolone 60-100 mg/day and nutritional support in severaly ill patients.
- Budesonide 4-8 mg daily, cortisone acting locally in intestine-no or little systemic actions.
III. Immuno-suppression
If the patient becomes cortisone dependent or refractory to treatment the same as in Crohn’s disease.
IV. Biological treatment
Infliximab be sure that the patient has no active TB.
V. Colectomy total with ileal pouch
How to Choose the appropriate treatment for UC?
The treatment aims to induce and maintain remission. This can be carried in a step-up or step-down approach depending on the severity of the disease.
For Induction of Remission
Mild-Moderate (step up)
- 1st line → 5 – ASA.
- 2nd line → Local steroids such as budesonide.
- 3rd line → systemic steroids as prednisone.
Moderate-Severe
- 1st line → Local steroids.
- 2nd line → systemic steroids as prednisone.
- 3rd line → immunosuppressive and biologics.
- Surgery.
For Maintenance of Remission
- Observation or 5-ASA following induction by 5-ASA or local steroids.
- Azathioprine following induction by systemic steroids.
- Immunosuppressive and biologics continued as maintenance if used for induction.
Treatment of toxic megacolon
- Stop pral feeding.
- Hospitalize the patient.
- Fluid and electrolyte balance.
- Broad spectrum antibiotics.
- Methyl predinsolone 100 mg/day.
- Prophylactic anticoagulation.
- If improved → maintain remission with a combination of immunosuppressive and biologic agents.
- If there is no improvement within 48 hours → Total colectomy.
- If rupture → Air under the diaphragm, peritoneal signs on abdomen Surgery.
Extraintestinal manifestations
A- Musculoskeletal manifestations
- Can be categorized as either axial or peripheral.
- The axial presents in the form of sacroiliitis. It is usually associated with HLAB27 and doesn’t correlate with the activity of the disease.
- The peripheral is either reactive-like or rheumatoid-like. Both aren’t associated with HLAB27 but correlate with the activity of the disease.
- The reactive-like type is asymmetric, monoarticular or oligoarticular, and migratory. The rheumatoid-like type is symmetric, polyarticular, and distal.
B- Oral manifestations
- Aphthous ulcers in Crohn’s disease.
- Hypertrophy of lips Crohn’s disease.
C- Ocular manifestations
Scleritis and uveitis (anterior) episcleritis with acute active disease are usually associated with erythema nodosum and HLA-B27.
D- Hepatobiliary
- Iry sclerosing cholangitis especially with UC. Its incidence is unaffected by colectomy.
- Peri cholangitis increases alkaline phosphatase and transaminases.
- Cholesterol gall stones in ileal disease due to decrease in bile salt pool.
E- Dermatologic manifestations
- Erythema nodosum in Crohn’s
- Pyoderma gangrenosum in UC.
- Clubbing of the fingers.
F- Renal manifestations
- Nephrolithiasis.
- Hydroureteronephrosis.
G- Hypercoagulability and Thromboembolic manifestations
H- lung disease (least common):
Asymptomatic decrease in diffusing capacity/to disabling bronchiectasis.
IBD and Malignancy
Incidence
IBD (either UC or CD) is associated with an increased risk o of colorectal carcinoma.
Risk factors tors for colorectal cancer in IBD
- The Anatomic extent of the disease.
- Duration of disease (most important).
- Age at onset of disease.
- Primary sclerosing cholangitis.
- Disease activity.
- Family history of colorectal cancer.
Surgery in UC
- Massive hemorrhage.
- Perforation.
- Fulminant colitis (Biological).
- No response to treatment (biological).
- Higher dose cortisone dependent (biological).
- Dysplasia or malignancy.
- Toxic megacolon.
Surgery for Crohn’s disease
- Strictures: balloon dilation or reconstruction.
- Fistulas (trial first with infliximab).
- Mass or abscess.
- Intestinal obstruction not responding to medical treatment.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach