Treatment of thyroid diseases in elderly, What are the causes of thyroid problems in the elderly?
Thyroid gland dysfunction is common in the elderly and is associated with significant morbidity if left untreated, Hypothyroidism occurs in 10% of females and 2% of males in patients older than 60 years, Hyperthyroidism, on the other hand, is more common in the younger population. The prevalence in the elderly is approximately 2%.
Thyroid function in normal aging
- The thyroid gland produces thyroxin (T4) and triiodothyronine (T3), With age, the thyroid gland undergoes moderate atrophy and develops nonspecific histo-pathologic abnormalities: fibrosis, increasing numbers of colloid nodules, and some lymphocytic infiltration.
- By age; Production of T4 decreases by about 30% due to decreased utilization of the hormone by tissue and not as a manifestation of primary thyroid failure.
- Decreases utilization of T4 correlates with the age-related decline in lean body mass, suggesting that the mass of metabolically active, protein-rich tissue (i.e., muscle, skin, bone, and viscera) decreases, which may lead to reduced use and catabolism of thyroid hormones.
Changes in hormonal levels
- Total Serum T3 and FT3 levels decrease moderately with age. This decline is thought to be due to decreased mono-deiodination of T4, The decline in serum T3 may be as much as 35%.
- The average serum TSH level rises with age, whether this change is a normal adaptive response associated with senescence or an actual increase in abnormal function is unclear.
Hypothyroidism
- Hypothyroidism occurs in 10% of females and 2% of males in patients ≥ 60 years.
- 3.1-8.5% of those ≥ 65 have subclinical hypothyroidism (isolated elevation of TSH levels with normal T4 and T3, with or without symptoms).
- The prevalence rises with age. women > men at all ages.
- The prevalence is higher in elderly patients in institutions than in community-dwelling elders.
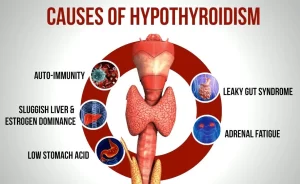
ETIOLOGY
Common causes:
- Hashimoto’s disease/ idiopathic.
- Previous irradiation.
- Surgical removal of the thyroid gland.
- After 1311 therapy for hyperthyroidism.
Less common cause:
- Pituitary and hypothalamic disorders.
- lodine-induced hypothyroidism.
- Transient hypothyroidism may occur after thyroid surgery, after treatment with radioactive sodium iodide (131I), or during episodes of subacute thyroiditis when the thyroid gland has depleted its store of hormone and the follicular cells have not yet recovered sufficiently to replace it.
Clinical picture
Elderly patients have significantly fewer symptoms of hypothyroidism than do younger adults and complaints are often subtle and vague. Chilliness, weight gain, muscle cramps, and paresthesias are significantly less common in patients ≥70 than in those ≤ 55. Fatigue, weakness, depression, constipation, and dry, coarse skin may also be less common.
Many elderly patients with hypothyroidism present with nonspecific geriatric syndromes: confusion, anorexia, weight loss, falling, incontinence, decreased mobility, arthralgias, and muscular aches.
Physical findings may be difficult to interpret.
- Puffiness around the eyes and myxedematous facies are difficult to distinguish from normal facial changes in elderly persons.
- Prolonged relaxation time after muscular contraction may not be detectable in older patients because of decreased amplitude or absent reflexes.
Occasionally, noninflammatory effusions may occur in the joints and pleural, pericardial, and peritoneal cavities.
Complications
- Hypertension.
- Dyslipidemia.
- CAD, MI, and HF due to elevation of lipoprotein.
- myxedema coma, a life-threatening emergency. Mental confusion progresses to stupor and coma and is often accompanied by hyponatremia, hypoglycemia, or hypercapnia.
Diagnosis
- The most sensitive indication of hypothyroidism due to primary thyroid gland failure is a marked elevation of serum TSH + subnormal serum-free T4 level.
- The serum T3 level has little value because it is normal in about one-third of patients with hypothyroidism and because subnormal levels are often due to illness or inadequate caloric intake.
Sub-clinical hypothyroidism
- Serum TSH level between 5-15 mU/L.
- The serum-free T4 level is at a low normal level.
- Thyroid antibodies have a prognostic value; the rate of progression to overt hypothyroidism is much higher in those with positive antibody titers.
Sick Euthyroid Syndrome
- It occurs in clinically euthyroid patients with severe non-thyroidal systemic illness.
- Findings may include low serum TT3 and FT3 levels and high serum reverse T3 levels.
- However, the difficulty arises because of low serum T4, free T4 index, and free T4 levels in the most seriously ill patients.
- So the diagnosis of hypothyroidism in the critically ill patient can be made only if the serum TSH level is markedly elevated (> 15 mU/L) or if the free T4 levels are markedly subnormal (< 0.6 ng/dL): hypothyroidism is more likely when both findings occur.
Screening
- Screening every 5 years by measuring serum TSH is recommended for all men ≥ 65 and all women ≥ 55.
- For those with risk factors for thyroid disease, the serum TSH level should be checked more often.
- Screening for hypothyroidism is as cost-effective as screening for hypertension, hypercholesterolemia, and breast cancer.
Treatment
Proper treatment of hypothyroidism completely corrects the metabolic condition. Long-standing, untreated hypothyroidism is a risk factor for coronary artery disease. Therefore, cardiac stress testing is indicated, and the response of blood lipid levels to treatment should be monitored.
The treatment of choice is T4 replacement with levothyroxine sodium (Eltroxin). The average dose for patients ≥ 65 years is 75 to 100 µg/day. If the patient has coronary artery disease, the initial dose of levothyroxine sodium should be only 12.5 to 25 µg/day.
Serum TSH level should be assessed after 1.5-2 months later. If the TSH level is still above normal, the dose may be increased by 25 µg. If the TSH is below normal (< 0.4 mU/L), the dose should be lowered. Serum FT3 and FT4 measurements usually are not needed.
If the serum TSH level is still high 1 to 2 months after reaching a dose of 100 µg/day of levothyroxine sodium, the dose should be maintained for another 2 months, If the TSH level is still elevated, the dose should be raised to 125 µg /day.
The physician should emphasize to the newly diagnosed patient with hypothyroidism that treatment with levothyroxine sodium must be maintained for life. This counsel should be repeated at follow-up visits at least once a year.
Treatment of myxedema coma
- large IV doses of thyroid hormones (eg, 200 to 500 µg levothyroxine sodium on the first day, then 100 to 300 µg IV on day 2, and 50 to 100 µg daily thereafter, until the patient can take oral levothyroxine.
- IV corticosteroids (hydrocortisone 50 to 100 mg q 6 h).
- Measures to treat hyponatremia, hypoglycemia, and respiratory failure, if present.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Histological structure of thyroid gland and Functions of Thyroid Hormones (T3 and T4)
Thyroid gland function, hormones, function, anatomy and Congenital anomalies
Posterior pituitary gland hormones & function, Control of ADH and Oxytocin hormone
Anterior pituitary gland function, hormones, location and Effects of Growth Hormone
Pituitary gland function, structure, location, hormones and anatomy
Endocrine system structure, function, disorders, Endocrine Glands and Hormone types