Staphylococci definition, diagnosis of staphylococcal infections and treatment
Staphylococcus is a Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales, Under the microscope, they appear spherical (cocci), and form in grape-like clusters. Staphylococcus includes at least 40 species, nine have two subspecies, one has three subspecies, and one has four subspecies, Many species cannot cause disease and reside normally on the skin and mucous membranes of humans and other animals.
Staphylococci
The genus Staphylococcus has at least 40 species. The three main species of clinical importance are Staphylococcus aureus, Staphylococcus epidermidis, and Staphylococcus saprophyticus. Staphylococci, particularly Staphylococcus epidermidis, are members of the normal flora of the human skin, respiratory tract and gastrointestinal tract. Nasal carriage of Staphylococcus aureus occurs in 25-50 % of humans.
Morphology
Staphylococci are Gram-positive spherical cells arranged in irregular clusters, They are non-motile and do not form spores.
Cultural characters
Staphylococci are facultative anaerobes, and grow readily on most bacteriologic media, Optimum temperature for growth is 37°C Staphylococcus aureus forms grey to golden yellow colonies and produces Beta hemolysis on blood agar. On mannitol salt agar, the selective medium for staphylococci, yellow haloes surround colonies of Staphylococcus aureus due to fermentation of mannitol with acid production Staphylococci are resistant to 10% NaCl.
Biochemical reactions
Staphylococci produce catalase which differentiates them from streptococci. Staphylococcus aureus is characterized by the production of coagulase which coagulates plasma, while other staphylococci are coagulase-negative. Staphylococcus aureus ferments mannitol with acid production.
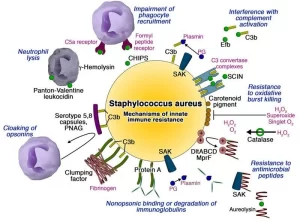
Virulence factors
The pathogenic capacity or virulence of a given strain of Staphylococcus aureus is the combined effect of structural factors & extracellular factors including toxins and enzymes.
A. Structural virulence factors
- Teichoic acid.
- Protein A.
- Clumping factor.
- Capsular polysaccharide.
Protein A is a cell wall component of Staphylococcus aureus strains, It has a strong affinity for the FC portion of the IgG molecule which becomes firmly bound to the staphylococcal cell wall, thus interfering with opsonization and phagocytosis.
Clumping factor (previously, bound coagulase) is a bacterial surface protein that binds fibrinogen converting it to insoluble fibrin which results in the protection of bacteria from phagocytosis by coating the organism with a layer of fibrin.
Due to the presence of a clumping factor, a suspension of Staphylococcus aureus forms clumps when mixed with plasma (principle of coagulase test), Most Staphylococcus aureus strains of clinical importance have polysaccharide capsules, which inhibit phagocytosis.
B. Enzymes and toxins
Catalase
Staphylococci produce catalase, which converts hydrogen peroxide into water and oxygen. Catalase test differentiates staphylococci, which are catalase positive, from streptococci, which are catalase negative. Bacteria that produce catalase can survive the killing effect of H₂O₂ within neutrophils.
Coagulase
Staphylococcus aureus produces coagulase which may deposit fibrin on the surface of staphylococci, hindering its ingestion by phagocytic cells.
Other enzymes
Include a hyaluronidase, or spreading factor, a/staphylokinase resulting in fibrinolysis, proteinases, lipases, and B-lactamase.
- Hemolysins: α-hemolysin lyses erythrocytes and damages platelets and smooth muscles.
- Panton-Valentine leucocidin (PVL): kills human leukocytes. It is an important virulence factor in community-acquired MRSA infections.
- Exfoliative toxins: these epidermolytic toxins yield the generalized desquamation of the staphylococcal scalded skin syndrome. The toxins are superantigens.
- Toxic shock syndrome toxin-1 (TSST-1): toxic shock syndrome toxin-1 (TSST-1) is a superantigen produced by most Staphylococcus aureus strains isolated from patients with toxic shock syndrome.
- Enterotoxins: there are multiple enterotoxins that are superantigens, The enterotoxins are heat stable and resistant to the action of gut enzymes, They are important causes of food poisoning, produced when Staphylococcus aureus grows in carbohydrate and protein food.
Virulence Factors in Staphylococcus
Mode of transmission of staphylococcal infections:
- Hands.
- Sneezing.
- Surgical wounds.
- Contaminated food: Custard pastries, Potato salad, Canned meats.
Clinical findings
A. Pyogenic infections
- Focal suppuration: folliculitis, impetigo, furuncles, carbuncles, breast abscess, cellulitis & postoperative wound infection.
- Disseminated infection: with visceral localization and suppuration. If Staphylococcus aureus disseminates and bacteremia follows, this can result in osteomyelitis and pneumonia. meningitis, empyema, lung abscess, brain abscess, and endocarditis. More than 50% of cases of Staphylococcus aureus bacteremia are acquired in the hospital after a surgical procedure or as a result of the continued use of a contaminated intravascular catheter.
B. Toxin-mediated illnesses
- Food poisoning: caused by staphylococcal enterotoxins. They behave as super antigens and their effect on the central nervous system results in severe vomiting within 3-6 hours of food consumption with rapid convalescence. The bacteria grow at room temperature and release toxins. Subsequent heating may kill the organism, but the toxin is stable.
- Toxic shock syndrome: is manifested by an abrupt onset of high fever, vomiting, diarrhea, myalgia, a scarlatiniform rash that desquamates (particularly on palms and soles), and hypotension with cardiac and renal failure in the most severe cases. Toxic shock syndrome associated with Staphylococcus aureus can be isolated from localized septic infections (e.g. wound infection), but virtually never from the blood stream i.e. there is no bacteremia 3-Scalded skin syndrome: due to exfoliative toxin causing generalized skin desquamation.
Coagulase-negative staphylococci (CONS)
The most important species of coagulase-negative staphylococci are Staphylococcus epidermidis and Staphylococcus saprophyticus. Coagulase-negative staphylococci are distinguished from Staphylococcus aureus by their negative reaction in the coagulase test.
A Staphylococcus epidermidis
Staphylococcus epidermidis is present in large numbers as part of the normal flora of the skin. Despite its low virulence, it is an important agent of hospital-acquired infections associated with the use of implanted prosthetic devices, such as heart valves, and catheters.
Staphylococcus epidermidis produces an extracellular polysaccharide material called polysaccharide intercellular adhesin (Sometimes called slime) that facilitates adherence to bioprosthetic material surfaces, such as intravenous catheters, and acts as a barrier to antimicrobial agents. Staphylococcus epidermidis is more often resistant to antimicrobial drugs than is Staphylococcus aureus, (75% methicillin-resistant).
B. Staphylococcus saprophyticus
This organism is a frequent cause of cystitis in women, probably due to its presence as a part of normal vaginal flora. Staphylococcus saprophyticus can be distinguished from Staphylococcus epidermidis and other CONS by its resistance to novobiocin.
Laboratory diagnosis of staphylococcal infections
Specimens
- Swabs or pus from cutaneous infections, wounds, and abscesses.
- Blood from cases of septicemia and bacteremia.
- Endotracheal aspirate, expectorated sputum, or CSF according to the localization of infection.
- Swabs from the anterior nares in case of screening for carriers to detect nasal colonization.
- In the case of food poisoning, often there are no viable organisms detectable in the consumed food, however enterotoxins can be detected by a latex agglutination test.
Gram-stained smear
Gram-stained smears often reveal Gram-positive cocci in clusters among pus cells. It is not possible to distinguish saprophytic from pathogenic staphylococci by smears.
Culture
Specimens inoculated on blood agar plates give rise to typical colonies in 18 hours at 37°C. Specimens contaminated with a mixed flora (vomitus, stool) can be cultured on mannitol salt agar.
- Blood agar plate may show a marked zone of β-haemolysis around Staphylococcus aureus colonies. Staphylococci produce pigmented colonies which vary in colour; golden yellow, lemon yellow, or white.
- Mannitol salt agar: the selective medium for staphylococci. The strain that ferments mannitol gives rise to colonies surrounded by yellow haloes, while non-mannitol fermenting colonies appear pink in colour.
The gram-stained film performed from culture reveals. Gram-positive cocci are arranged in irregular clusters. Colonies are further identified by their biochemical reactions.
Biochemical reactions
- Catalase test: All staphylococci are catalase positive. This test differentiates staphylococci from streptococci (refer to the practical section).
- Coagulase test: Staphylococcus aureus is coagulase positive. This test differentiates Staphylococcus aureus from both Staphylococcus epidermidis and Staphylococcus saprophyticus (refer to the practical section).
- Mannitol fermentation: Staphylococcus aureus ferments mannitol with acid production, Other Staphylococcus species do not ferment mannitol.
- Novobiocin test, Staphylococcus epidermidis is novobiocin sensitive while Staphylococcus saprophyticus is novobiocin resistant.
Susceptibility testing
Disc diffusion susceptibility testing should be performed routinely on staphylococcal isolates.
Detection of carriers
In Staphylococcus aureus hospital outbreaks, it is critical to define the carrier who initiated the outbreak. In tracing the source of infection, suspected patients, hospital staff, or food handlers are tested for the possibility of being nasal or skin carriers of the strain causing either the hospital epidemic or food poisoning. The isolated strains are subjected to typing in specialized laboratories.
Treatment
Serious Staphylococcus aureus infections require aggressive treatment including incision and drainage of localized lesions, removal of the device (prosthesis) as well as systemic antibiotics. More than 90% of Staphylococcus aureus strains contain plasmids that encode B-lactamase (conferring resistance to penicillin).
This has required the use of B-lactamase-resistant penicillins (e.g. methicillin or oxacillin). However, increased use of methicillin and related antibiotics has resulted in the emergence of methicillin-resistant Staphylococcus aureus (MRSA) 65% of all Staphylococcus aureus). MRSA: These strains are considered resistant to all beta-lactam antibiotics including penicillins, cephalosporins, and carbapenems.
Vancomycin is the agent of choice for the empiric treatment of life-threatening MRSA infections. Recently, the incidence of vancomycin resistance has increased steadily with the emergence of vancomycin-resistant Staphylococcus aureus (VRSA) promoting the use of alternative drugs such as linezolid. Strains of Staphylococcus aureus which are susceptible to methicillin (methicillin-sensitive Staphylococcus aureus (MSSA) are also susceptible to cephalosporins and other beta-lactams.
You can follow science online on YouTube from this link: Science online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Antibacterial agents types, Effect of Antibacterial Drugs and How do antibiotics work?
Microbiology, Bacteria structure, types, Gram-positive bacteria and Gram-negative bacteria