Small Intestinal Tumors, Risk factors for developing small intestinal cancers
The small bowel is the least common site for primary cancer. The small bowel contains more than 90% of the mucosal surface area of the GI tract, but only constitute 1.1-2.4% of all GI primary malignancies. The incidence of small intestinal tumors decreases from duodenum to ileum.
Benign Small Intestinal Neoplasms
Benign neoplasms account for 30-50% of small bowel tumors. These lesions are most frequently encountered in the duodenum as incidental findings during endoscopic examination.
1. Adenomas:
Adenomas are the most common neoplasm of the small intestine. Mostly encountered in the duodenum. Adenomas has different types that include
- Tubular adenoma: low malignant potential, pedunculated and present by bleeding, endoscopic polypectomy is the treatment of choice.
- Villous adenoma: sessile lesion with high malignant potential, mostly encountered in the peri-ampullary area.
Management:
A. Benign lesion: Endoscopic polypectomy, Surgical local excision.
- open the duodenum.
- inject adrenaline and saline
- circumferential around the Villous adenoma to elevate mucose from the muscosa and start restriction of the Villous adenoma.
B. Malignant tumors: Extensive major resection (pancreaticoduodenectomy)
- remove part of stomach + duodenum + jujuneum.
- gall bladder + head of the pancreas.
- lt is only for curative
- If there is metastasis behind you should not do this but palliative surgery.
Tubovillous adenoma: like villous adenoma.
Bruners gland hyperplasia: hyperplasia of the gland of the first part of the duodenum, benign condition, treated by endoscopic polypectomy.
2. Hamartomas
Small intestinal hamartoma usually is a part of:
- Peutz-Jeghers syndrome.
- Familial intestinal hamartomatous polyposis is characterized by multiple polypi in the jejunum and ileum (25% gastric and 50% colonic).
- Melanosis of oral mucous membrane, lips as well as palmer and planter surface intermittent intussusception and bleeding.
- Rare malignant potential increases the incidence of ovarian, breast, endometrial, and pancreatic tumors.
- Treated by surgical resection or endoscopic polypectomy.
3. Hemangiomas:
- Present by bleeding, occult or overt.
- Diagnosed and treated by selective angiography, and surgical resection.
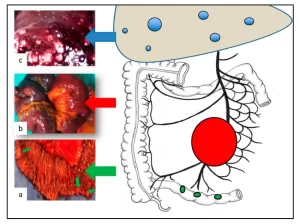
Small Intestinal secondaries
The small bowel is frequently affected by metastases either from direct extension (local invasion by cancers), intraperitoneal carcinomatosis, or hematogenous spread.
Common primary malignancies that can give small intestinal metastasis include malignant melanoma (commonest)) ovarian, bladder, breast or lung cancer.
Risk factors for developing small intestinal cancers:
- Ingestion of smoked or cured foods.
- consumption of red meat.
- celiac sprue.
- crohn’s disease.
- Peutz-Jeghers syndrome.
- hereditary non-polyposis colorectal cancer.
- familial adenomatous polyposis (FAP).
- AIDS.
1. Adenocarcinoma:
- Most common
- Villous adenoma.
- 40% in the duodenum − Periampullary lesions.
- Mean age 60.
- Sex 2:1 male predominance.
FAP and Adenocarcinoma
- Patients with FAP have a nearly.
- 100% cumulative lifetime risk of developing.
- duodenal adenomas that have the potential to undergo malignant transformation.
- The risk of duodenal cancer in these patients is over 100-fold that in the general population.
- Duodenal cancer is the leading cause of cancer-related death among patients with FAP who have undergone colectomy.
Crohn’s disease and Adenocarcinoma
- Patients with Chron’s disease have a 12-fold increased risk of small bowel cancer than the normal population.
- Adenocarcinoma developing in Chron’s disease is most found in the ileum and symptoms often mimic symptoms of Crohn’s.
- Risk factors for developing adenocarcinoma in a patient with Chron’s disease include: long duration of disease, male gender, fistulas, surgically excluded loops of small bowel, strictures, and immunosuppressive drugs.
Management:
For adenocarcinomas, a wide resection (5 cm of the distal and proximal margin) and anastomosis of the segment harboring the tumor with wide excision of the corresponding mesentery are performed to achieve regional lymphadenectomy. The continuity of the small bowel is then restored by anastomosis.
Right hemicolectomy: This is done exclusively for adenocarcinomas of the distal ileum. Pancreaticoduodenectomy for duodenal tumors. In the presence of locally advanced or metastatic disease, palliative intestinal resection or bypass is performed:
- gastrojejunostomy and choledoco jejunostomy.
- Endoscopic Wall stent placement for duodenal obstruction and bile stent placement for obstructive jaundice.
- Alcohol neurolysis (Chemical splanchnicectomy) for pain control.
- Localized disease 80% long-term survival, advanced disease 10-15%, 5-year survival.
Chemotherapy has no proven efficacy in the adjuvant or palliative treatment of small Intestinal Adenocarcinomas.
Prognosis
- Localized disease: 80% long-term survival.
- Advanced disease: 10%-15% five-year survival.
2. Carcinoid Tumors:
- Arise from Kulchitsky cells in the crypts of Lieberkuhn (ECL cells) -(Neuroendocrine cells (APUD system).
- Secrete several endocrine and vasoactive peptides e.g. Serotonin, Substance P, Dopamine, Histamine, Prostaglandins E&F.
- 85% occur in the appendix, ileum, and rectum in order of frequency.
- 30-40% have multiple synchronous lesions in the jejunum.
- Metastasize to the liver, Carcinoid syndrome: Reddish blue cyanosis, flushing attacks, diarrhea, asthmatic attacks, pulmonary and tricuspid stenosis, Rt-sided ht. failure.
- Diagnosis by the demonstration of the increased level of 5-HIAA in urine.
- Non-carcinoid synchronous tumors are found in up to 25% of patients (typically tumors of the breast, lung, stomach, or colon).
- Approximately 25 to 50% of patients with carcinoid tumor-derived liver metastases will develop manifestations of the carcinoid syndrome.
Management:
Most asymptomatic discovered incidentally.
Treatment:
- For small bowel: surgical resection.
- For the appendix: appendicectomy (appendectomy).
- Metastatic disease: enucleation or liver resection.
- Somatostatin analogue: Octreotide. Slowly growing.
3. Small Intestinal GISTS
- The terms leiomyoma and leiomyosarcoma have been replaced by a more general term, gastrointestinal stromal tumor (GIST).
- The theory is that GISTs arise from the interstitial cell of Cajal an intestinal pacemaker cell.
- GISTs may have myogenic features, neural features or both or they may lack differentiation.
- They can present with benign or malignant characteristics.
Important markers of prognosis
- Tumor size.
- Mitotic activity.
- Spread of the disease outside the bowel wall.
- Poor histological grade.
- Short time from symptoms to diagnosis.
Tumor markers
- CD 117
- CD 34
Management of Small Intestinal GIST
- Surgical resection of the entire tumor, along with local extensions and localized peritoneal or liver metastases, is the treatment of choice.
- Segmental intestinal resection if the diagnosis is known before resection, wide lymphadenectomy can be avoided as GISTs are rarely associated with lymph node metastasis.
- GISTs are resistant to radiotherapy and chemotherapy, their role in adjuvant treatment is not defined.
- The specific treatment of GIST is Tyrosine Kinase inhibitor (Gleevec) Imatinib which is used with those with advanced or metastatic disease.
4. Small Intestinal Lymphomas
- Lymphoma may involve the small intestine primarily or as a manifestation of disseminated systemic disease.
- Primary small intestinal lymphomas are most commonly located in the ileum, which contains the highest concentration of lymphoid tissue.
- Although partial small bowel obstruction is the most common mode of presentation, 10% of patients with small intestinal lymphoma present with bowel perforation.
- Primary Gl lymphomas are the most common of extra nodal lymphomas (5% of all lymphomas).
- They present as primary neoplasms without systemic nodal disease or as secondary tumors as a part of disseminated lymphoma.
- Most are Non-Hodgkin’s B-cell lymphomas with intermediate or high-grade features.
What defines primary lymphoma of the gut?
- Absence of peripheral.
- lymphadenopathy.
- Absence of mediastinal.
- lymphadenopathy.
- Normal white blood cell count.
- Absence of bone marrow lymphoma.
- At laparotomy, the disease is restricted to the bowel and proximal lymph nodes with no involvement of the liver or spleen.
Risk factors associated with an impaired mucosal barrier
- Malabsorptive or inflammatory conditions e.g. celiac sprue, Crohn’s disease.
- Helicobacter pylori infection→ small bowel lymphoma.
- Immunosuppressed patients due to:
- Pharmacological e.g. post-transplant immunosuppressants e.g. cyclosporine.
- HIV infection (AIDS): Gl lymphomas (B-cell non-Hodgkin’s lymphoma) and Kaposi’s sarcoma can appear in any organ.
- Diseases that cause immunological dysfunction e.g. rheumatoid arthritis.
- Congenital e.g. agammaglobulinemia and congenital immunodeficiency syndrome.
Different types of primary intestinal lymphoma:
They are Non-Hodgkin’s lymphoma, mainly of the B cell type.
Mature (peripheral) B-cell:
- Extra nodal Marginal Zone B-cell lymphoma→ (MALT Type).
- Diffuse large B-cell→ High-grade and MALT type.
- Mantle cell.
- Burkitt’s lymphoma.
- Mature T-cell→ Enteropathy type T-cell (EATCL).
Management of Small Intestinal Lymphomas
- Localized small intestinal lymphoma should be treated with segmental resection of the involved intestine and adjacent mesentery.
- If the small intestine is diffusely affected by lymphoma, chemotherapy) rather than surgical resection should be the primary therapy.
- Surgical resection in stage 1 or II, debulking for large complicating tumors in stage III or IV.
- All patients receive chemotherapy.
- The role of radiation therapy is unclear.
The prevalence of small bowel tumors identified at autopsy is 0.2-0.3%, which is significantly higher than the rate of operation for small bowel tumors. This suggests that the majority of small bowel tumors are asymptomatic.
The Most Common Signs and Symptoms of Small Intestinal Neoplasms:
- Abdominal pain, 67%.
- Progressive: malignant.
- Intermittent: benign.
- GIT bleeding (occult, melena or manifest 41%.). Slow: hemangioma or adenoma. Significant: GIST
- Weight loss, 38%.
- Nausea and vomiting, 33%.
- Bowel obstruction, 13%.
- Intussusception, in adults (benign).
- Malabsorption (lymphoma).
- Palpable mass, 7 18% (GIST).
- Perforation, 25% (lymphomas).
- Painless jaundice (periampullary carcinoma.
- Decreased appetite.
Diagnosis of Small Intestinal Neoplasms
1. Plain radiographs:
- intestinal obstruction (multiple air-fluid levels but need further investigations to know the cause of obstruction.
- Calcified abdominal masses.
2. Contrast (Barium) Radiography of the Small Intestine:
- Contrast radiography of the small intestine may demonstrate benign and malignant lesions.
- Enteroclysis (small bowel enema, normally administered through a nasogastric tube).
- is reported to have a sensitivity of over 90% in the detection of small bowel tumors and is the test of choice, particularly for tumors located in the/distal small bowel.
- Upper Gl with small bowel follow-through examinations have reported sensitivity of only 30% -44%.
3. CT scan:
- CT scan has a low sensitivity for detecting mucosal or intra-mural lesions, but can demonstrate (large tumors and is useful in the staging of intestinal malignancies.
- Sensitivity depends on tumor location 100% in the duodenum, 17% in the jejunum, and 70% in the ileum.
- CT enteroclysis (helical CT with enteroclysis).
- Useful in the staging of intestinal malignancies.
4. Endoscopic Studies – Biopsy
- Upper GIT Endoscopy: Tumors located in the duodenum can be visualized and biopsied on upper Gl endoscopy.
- Endoscopic ultrasonography can offer additional information such as the layers of the intestinal wall involved in the lesion.
- Intra-operative enteroscopy: It can be used to directly visualize small intestinal tumors beyond the reach of standard endoscopic techniques.
- Colonoscopy: It can occasionally visualize the distal ileum successfully.
- Recently, capsule endoscopy and double-balloon endoscopy have been used to evaluate small bowel.
5. Bleeding scan and angiography
- Tumors associated with significant bleeding can be localized with angiography or radioisotope-tagged RBC scans.
- Angiography: rapid bleeding 0.3-0.5 ml/min.
- Bleeding scan (Technetium-labeled RBC scan): slow bleeding > 0.1 ml/min.
Notes: If there is jaundice start with ultrasound then MRI next CT. IF obstruction use Plain radiographs.
6. Lab investigations:
- Laboratory tests are non-specific, except for elevated serum 5- hydroxyindole acetic acid levels in patients with carcinoid syndrome.
- Elevated CEA levels are associated with small intestinal adeno-carcinomas, but only in the presence of liver metastases.
- CD117 and CD34→ GIST
Treatment:
Benign:
- Surgical resection or endoscopic polypectomy.
- Villous adenoma → Whipple’s operation.
Adenocarcinoma:
- Resected with 5 cm + wide excision of the mesentery.
- Distal ilium → R.T hemicolectomy.
- Duodenal tumors→ Whipple’s
- Palliative surgery.
Carcinoid:
- Appendectomy.
- Octreotide.
GIST:
- Segmental intestinal resection…rarely affects LNs.
- Imatinib.
Lymphoma:
Localize→ Segmental intestinal resection of the involved intestine + adjacent mesentery
Diffuse→ Chemotherapy + debulking of stage 3 or 4
If there is metastatic palliative or bypass and there is no radical or curative for that legion.
prognosis of malignant small bowel tumors
- Overall survival of patients with small bowel malignancies is poor.
- Adenocarcinoma: Periampullary, 30-40% 5-year survival rate,
- elsewhere <20%,
- GISTS: 30-40% 5-year survival rate.
- Lymphoma: 10-50% 5-year survival rate.
- Carcinoid: 75% for local tumors, 19% for tumors with distant metastases.
You can follow Science Online on Youtube from this link: Science online
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut & hindgut
Histological structure of stomach, Fundic glands of Stomach & Gastric musculosa
Abdomen muscles, Blood Supply of Anterior Abdominal Wall & Rectus Sheath content
Large Intestine function, parts, length, anatomy & Relations of the rectum
Pancreatic secretion composition, regulation, function, Differences between jejunum & ileum