Risk factors for falling, Preventing falls in the elderly and Effective Interventions to Reduce Falls
There are many risk factors for falling, Falling, especially in older adults can lead to serious injuries such as fractures, head injuries, or death. Various risk factors contribute to an increased likelihood of falling, which can be grouped into physical, environmental, and lifestyle-related factors.
Physical Risk Factors
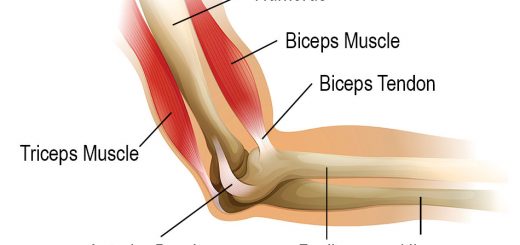
- Reduced strength in the legs or lower body increases the chance of losing balance.
- Poor balance and difficulties walking or with coordination increase the risk of falling.
- Impaired vision, due to cataracts or glaucoma, can make it harder to navigate safely.
- Painful feet or inappropriate shoes can hinder stable walking.
Chronic Health Conditions
- Neurological conditions such as Parkinson’s, stroke, or multiple sclerosis.
- Cardiovascular issues (such as low blood pressure causing dizziness).
- Diabetes can lead to neuropathy or loss of sensation in the feet.
- Certain medications (e.g., sedatives, antidepressants, antihypertensives) can cause dizziness or drowsiness.
- A drop in blood pressure when standing up can cause lightheadedness and falls.
- Conditions such as dementia can affect judgment and awareness, leading to falls.
- Depression may be associated with lower energy levels and physical activity, leading to muscle weakness.
- Anxiety about falling may lead to reduced physical activity, which can weaken muscles and increase the risk of a fall.
Environmental Risk Factors
- Loose rugs, uneven flooring, poor lighting, or items left in walkways can cause tripping.
- Lack of handrails or poorly lit stairways can increase fall risk.
- Wet or waxed floors, especially in bathrooms or kitchens, can lead to slipping.
- Poor Lighting: Inadequate lighting makes it harder to see obstacles and increases the risk of tripping.
Lifestyle and Behavioral Risk Factors
- Lack of physical exercise weakens muscles and affects coordination and balance.
- Alcohol Use: Excessive alcohol consumption can impair judgment, coordination, and reaction times.
- Using walkers, canes, or other devices incorrectly can lead to falls.
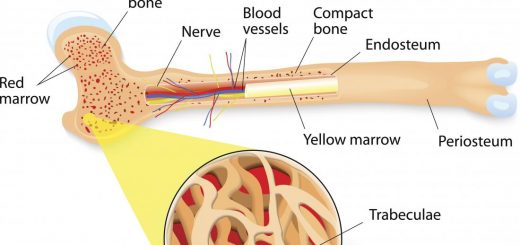
- Poor diet can lead to muscle weakness, fatigue, or poor bone health (e.g., osteoporosis).
Preventative Measures
- Strengthening exercises and balance training.
- Regular eye exams.
- Evaluating medications with healthcare providers.
- Ensuring the home environment is safe (adding grab bars, improving lighting, removing clutter).
- Using assistive devices such as those recommended by health professionals.
Risk factors for falling
- Age greater than 80 years.
- need for assistance with activities of daily living.
- previous falls (check circumstances of the fall risk for future fills).
- these characteristics cannot be modified, they serve as indicators for clinicians to pay increased attention to the presence of other, treatable risk factors for falls.
- Vision is affected by age, impaired contrast sensitivity (the ability to detect edges), and depth perception. Multifocal lenses, are commonly worn by presbyopic older persons.
- Hearing loss & impaired vestibular function can lead to loss of balance when there is decreased visual input.
- Proprioceptive dysfunction can result in loss of balance on uneven ground or in situations, such as walking in the dark, where there is decreased visual input.
- Dementia.
- Depression.
- Postural Hypotension: A of drop in systolic blood pressure of 20 mmHg or more with a change in position from lying to standing.
- Postprandial hypotension may be suspected in persons complaining of dizziness or who fall after getting up from, or soon after, a meal.
- Musculoskeletal Impairments: Muscle mass and strength decline with age, disease, and inactivity. Foot problems, such as calluses, bunions, long nails, or joint deformity.
- Review other systems (chest, heart,…).
- Medications: The number of drugs taken is an independent risk factor for falls even if OTC drugs. The use of four or more prescription and non-prescription medications increases the risk of falling. The type of drug is another factor e.g anticonvulsant, sedative, hypnotics, anti-depressants and benzodiazepines. In addition, antiarrhythmic medications, antihypertensives, digoxin, and diuretics.
- Acute Illness and Hospital Discharge: Acute illness, such as pneumonia or exacerbation of congestive heart failure, may present as a fall in a frail older person. The risk of a fall in older persons recently discharged from the hospital and receiving home care is about fourfold higher than that for others in the community during the first 2 weeks after discharge. Extrinsic risk factors for falls include environmental hazards.
Screening for fall risk
- All older persons seen for routine medical care should be screened for fall risk by asking, at least once a year, if they have fallen.
- They should be observed getting up from a chair and walking across a room for difficulty with the activity, unsteadiness, or use of an assistive device (Timed Up and Go Test).
- routine vision and hearing screening.
- regular review and reduction, when possible, of medications.
- screening for and treatment of osteoporosis.
- exercise prescription (bone & muscle mass responds well to exercise even in the oldest age ranges.
- discussion of home safety.
Timed UP & GO test
- The patient is seated on a hard sturdy chair.
- Stand up.
- Walk 3 meters at this usual walking pace.
- Turn 180 degrees.
- Walks back to the chair.
- Sets down
- Normally adults take about 9 to 12 Seconds.
- More than or equal to 14 Seconds = Increased risk.
If there is a history of one or more falls, (significant fall, more than twice in six months or once but associated with injury), or if the person has problems with mobility or gait, then a more detailed fall risk assessment is needed.
Multifactorial assessment Routinely conducting an in-depth multifactorial risk evaluation and comprehensive management of identified risks of falls are not recommended. This strategy may be beneficial only to selected patients, depending on, the circumstances of previous falls and comorbidities.
Preventing falls in the elderly
Effective Interventions to Reduce Falls
- Effective exercises: minimum 10 weeks effective even in very old individuals. individualized to be effective in fall prevention. Group exercises include Tai Chi exercises and others. It is recommended that older adults get at least Moderate-intensity 30 min. 5 times a week. Nice Guidelines, It is recommended AGAINST brisk walking as it increases fall risk in the elderly.
- Older persons can also be taught how to get up from the floor to prevent a long lie as a result of a fall.
- De-prescribing strategy: Gradual withdrawal and modification of drug prescription.
- Safety modifications in the home.
- Diminish the impact of the fall.
- Parkinsonian: Retropulsion… squatting.
- Walking cane: external rotation.
- Medical alert system: Wear a pendant alert device with a help button built-in to it. If an emergency, simply press the help button and the emergency monitoring center will pick up the signal. The emergency personnel can speak with the elderly through the microphone on the base station. They will assess the situation and dispatch the appropriate responders. The mobile system also offers GPS tracking technology so that responders can find the elderly no matter where he is.
- Home environment: floors, lighting, stairways, bathroom and kitchen.
- Other effective strategies for older persons:
- Hip protectors (shock absorber).
- Zimmer frame.
- Medical alert system.
- Treatment osteoporosis.
Interventions NOT effective in Reducing Falls
- In general, vitamin D supplementation did not lower fall rate, unless it was given to the elderly to correct vit D deficiency.
- Education regarding fall prevention also did not lower the fall rate.
- routinely conducting an in-depth multifactorial risk evaluation and comprehensive management of identified risks of falls are not recommended.
- This strategy may be beneficial only to selected patients, depending on. circumstances of previous falls and comorbidities.
How to use walking canes correctly?
- proper height: handle of the cane at the level of the greater trochanter.
- during walking: the cane should be held in the hand opposite to the side of the diseased leg.
- climbing upstairs: Both hands must be supported patient goes up with the Good leg first.
- going downstairs: Both hands must be supported patient goes down with the diseased leg first.
Note that the main aim in managing falling problems is to keep the patient moving but in a more safe situation. We do not restrict activity unless clearly hazardous situation (e.g. climbing over a chair to reach too high objects should be avoided). This is important since restriction of activity would lead the patient to immobility. (Immobility in itself has its serious complications.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Causes of Falls in the elderly, How to prevent falls and Why do the Elderly die after a fall
Urinary incontinence in elderly causes and treatment, How to correct urinary incontinence?
Properties of cardiac muscles, Cardiac automaticity, and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure, and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk, and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart and Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function