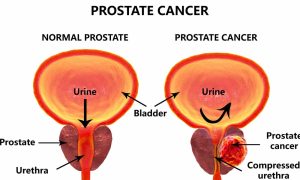
Prostate function, structure, lobes, Benign enlargement of prostate and malignant prostatic tumor
The prostate is a firm partly glandular and partly fibro-muscular organ. It is in the pelvic cavity, between the lower border of the symphysis pubis anteriorly and the ampulla of the rectum posteriorly. It is conical in shape and presents a base, an apex, and an anterior, posterior, and 2 lateral surfaces.
Prostate
The base of the prostate is directed up, surrounds the neck of the urinary bladder, and is penetrated by the urethra, The apex is directed down, and in direct contact with the superior fascia of the urogenital diaphragm. The posterior surface lies in direct contact with the ampulla of the rectum and can be palpated by perrectal (P/R) examination in the living.
The anterior surface is connected to the pubic bone by the puboprostatic ligament. The urethra emerges from this surface above and in front of the apex of the gland. Inferolateral surfaces (one on each side):
- Related to the 2 free borders of the levator ani muscle. The most anterior part of this muscle (Levatore prostate).
- Passes backwards from the pubis and embraces the sides of the prostate to reach the perineum body.
Structures inside the prostate
- Prostatic urethra; pierced by the ducts of the prostatic acini and by the 2 ejaculatory ducts.
- The ejaculatory ducts, run down and forwards one on each side to open into the prostatic urethra.
- Prostatic utricle: extends upwards and backwards from the prostatic urethra into the median lobe.
Lobes of the prostate
Anatomical lobes:
- The median lobe lies behind the prostatic urethra and is bounded by an ejaculatory duct on each side. It projects up behind the internal urethral orifice to form the uvula of the bladder.
- Right and Left lateral lobes: lie on each side of the prostatic urethra.
- The anterior lobe (isthmus) connects the lateral lobes in front of the urethra and contains little glandular tissue.
- Posterior lobe.
Prostatic capsule
- Inner true capsule: a firm fibromuscular adherent to the prostate substance.
- Outer false capsule (prostatic sheath): formed by pelvic fascia.
- Prostatic venous plexus is: situated between the 2 capsules.
- The arterial supply: inferior vesical and middle rectal arteries.
- Venous drainage: prostatic venous plexus. Drains into the internal iliac vein. The prostatic venous plexus is also connected to the vertebral venous plexus by valveless veins (this is how prostate cancer spreads to the vertebrae).
- Lymph drainage: sacral and internal iliac lymph nodes.
Histological structure of the prostate
It is composed of the following
- Connective tissue stroma is formed of fibro-elastic connective tissue capsule containing smooth muscle fibers and dense fibro-elastic connective tissue septa between the acini which are also rich in smooth muscle fibers.
- Secretory acini: prostate is a compound tubuloalveolar (acinar) gland. The glandular acini of the prostate is embedded in the dense stroma.
Prostatic acini are irregular in outline and lined by simple columnar epithelium. occasionally patches of simple cuboidal, squamous, or pseudostratified columnar epithelium are present.
Histologically and clinically, the prostatic acini are arranged into 3 concentric layers (zones) as follows:
1. Mucosal glands
- Central in position (periurethral) and small in size.
- Secrete directly into the urethra.
2. Submucosal glands:
- Medium-sized.
- Secrete into the urethra by short ducts.
3. Outer (main) glands:
- Large and numerous.
- Secrete into the urethra by long ducts.
Prostatic concretions (corpora amylacea)
In older men, the precipitation of the secretory material occurs inside the lumen of some acini forming lamellated structures which may become calcified.
Functions of the prostate gland
- Secretion of thin, milky fluid, rich in glycoproteins and prostaglandins, forming a considerable part of semen.
- The secretion contains enzymes eg. acid phosphatase and protease that liquefies coagulated semen after ejaculation.
Clinical notes:
Benign enlargement of the prostate (Benign prostatic hyperplasia (BPH) is common in men older than 50 years (senile enlargement). It is present in about 95% of men above 70 years of age. Prostatic acini of mucosal and submucosal glands are involved in this disease.
The median lobe of the gland enlarges upward and encroaches within the sphincter vesicae, located at the neck of the bladder, The leakage of urine into the prostatic urethra causes an intense reflex desire to micturate, The enlargement produces a distortion of the urethra so that the patient experiences difficulty in passing urine and the stream is weak.
The enlargement of the uvula vesicae (owing to the enlarged median lobe) results in the formation of a pouch of stagnant urine behind the urethral orifice within the bladder. The stagnant urine frequently becomes infected, and the inflamed bladder (cystitis)) adds to the patient’s symptoms.
The malignant prostatic tumor is the second most common cancer in men. Prostatic acini of the outer group are involved in this disease.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Organs of male genital system, Structure of the testis, Functions of Sertoli cells & Leydig cells
Testis functions, sperms production, Factors affecting spermatogenesis, Structure of Epididymis
Vas deferens function, histology, anatomy, Varicocele & Functions of Seminal vesicle
Testosterone effects, low testosterone symptoms, Hypogonadism & Hypergonadism in male