Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Portal venous system can drain blood from the gastrointestinal tract (apart from the lower section of the rectum), spleen, pancreas, and gallbladder to the liver, It is formed from the 4th to the 12th gestation week, developing from the vitelline venous system in close relation with the umbilical venous system.
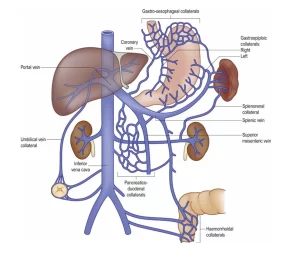
The Portal Venous System
- It is the system formed by the veins draining the GIT.
- These veins collect into the portal vein which breaks into the liver sinusoids.
Portal vein
Origin: It is formed by the union of the superior mesenteric and splenic veins behind the neck of the pancreas and in front of IVC.
Course & relations: It ascends behind the 1st part of the duodenum and in front of IVC, then in the free border of the lesser omentum with both the hepatic artery (left) and bile duct (right) anterior to it, It is separated from IVC by the epiploic foramen, Then it terminates in the porta hepatis where it divides into right and left branches.
Tributaries
- Superior mesenteric vein.
- Splenic vein (It receives the inferior mesenteric vein).
- Right gastric vein.
- Left gastric vein.
- Paraumbilical vein (in the left branch) of the portal vein.
- Cystic vein (in the right branch) of the portal vein.
The inferior mesenteric vein terminates in the splenic vein.
Portosystemic anastomosis
- These are the sites where veins belong to the portal venous system anastomose with veins belong to the systemic circulation.
- They are important surgically because in case of liver cirrhosis, the pressure in the portal vein and its tributaries increases. The anastomotic veins will be enlarged, tortuous and engorged with blood and it will shift from the portal veins to the systemic circulation.
Sites of portosystemic anastomosis
- At the lower end of oesophagus, Portal vein: Left gastric vein, Systemic vein: Azygos vein, Effect: Oesophageal varices haematemesis.
- At the end lower of the anal canal, Portal vein: Superior rectal vein, Systemic vein: Middle, inferior rectal veins, Effect: Rectal varices Piles (haemorrhoids) —-> bleeding per rectum.
- Around the umbilicus, Portal vein: Left br. of portal Vein, Systemic vein: Veins of ant. Abdominal wall, Effect: Caput meduosa.
- Anastomosis between the right colic vein (portal) and the right renal vein. (systemic). (the same on the left side).
- Anastomosis between the bare area of the liver (portal) and the phrenic veins (systemic).
- Anastomosis between the superior mesenteric vein (portal) and the IVC (systemic).
Histological structure of the liver
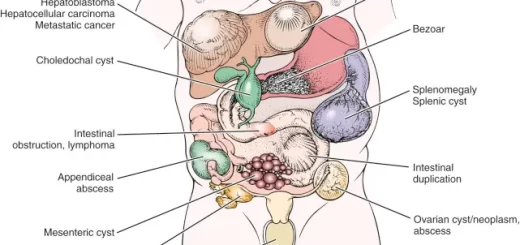
The liver is the largest gland and the main metabolic organ of the body. Unlike the pancreas in which the mixed exocrine-endocrine function is carried out by two distinct components, the dual function of the liver resides in the same cell, the hepatocyte.
Histological organization of the liver
It is a compound tubular gland with unique histological organization and microvasculature, constructed of the following:
I- The hepatic stroma
The liver is surrounded by a thin connective tissue Glisson’s capsule which is partially covered by mesothelium. The capsule becomes thicker at the hilum (porta hepatis), where the connective tissue septa arise and the portal vein and hepatic artery enter the liver, while the right and left hepatic ducts and lymph vessels exit.
The connective tissue of interlobar septa is not apparent in the human liver but is evident in the liver of the pig. Network of reticular fibers that support the hepatocytes and the blood sinusoids.
II- The hepatic parenchyma
The parenchyma of the liver consists of anastomosing cords of hepatocytes arranged in the form of plates of cells radiating from a small central vein. These hepatic cords enclose between them narrow bile canaliculi and are separated from each other by blood sinusoids.
Histological features of hepatocytes
- They are polyhedral cells having a rounded, centrally-located euchromatic nucleus. Some hepatocytes are binucleated.
- The cytoplasm is eosinophilic (due to the presence of large numbers of mitochondria and abundant SER for the synthesis of bile & glycogen and detoxification of drugs) and pale (due to the presence of glycogen granules and lipid droplets).
- Abundant rER with multiple Golgi complexes for synthesis and secretion of various plasma proteins and lipoproteins.
- Numerous peroxisomes for oxidation of fatty acids.
- Many lysosomes and lipofuscin pigments.
- The hepatocyte has two important functional surfaces:
- The vascular side faces the perisinusoidal space. It shows long numerous microvilli, which increase the surface area.
- The intercellular side where bile canaliculi are enclosed between adjacent hepatocytes. Each bile canaliculus shows short microvilli projecting into its lumen which is bounded by tight junctions and desmosomes.
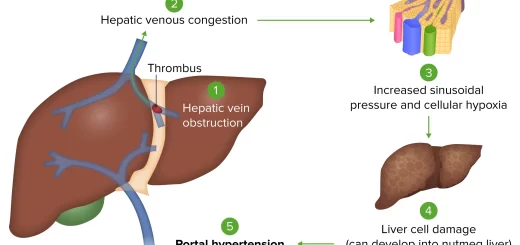
III- The hepatic blood sinusoids
The liver has a double blood supply, receiving oxygenated blood from the general circulation via the hepatic artery (25%) and a large amount of poorly-oxygenated blood but rich in nutrients coming from the intestinal tract via the portal vein (75%).
On entering the porta hepatis the portal vein and the hepatic artery branch repeatedly and give off interlobular branches, running in the portal canals between the hepatic lobules, they pour their mixed blood into the hepatic sinusoids.
The hepatic blood sinusoids carry a mixture of arterial and portal venous blood, where blood is directed to the center of the classic hepatic lobule to drain into the central vein. Central veins from each lobule converge into larger veins and eventually form the hepatic veins to end in the inferior vena cava.
Hepatic blood sinusoids form an anastomosing plexus between the cords of hepatocytes, presenting an enormous surface area for the exchange of metabolites between the blood and the hepatic parenchyma. The hepatic sinusoid is lined by two types of cells:
- Fenestrated endothelial cells: flat cells with numerous large fenestrations without diaphragm and surrounded by a thin discontinuous basal lamina. This allows free passage of plasma into the perisinusoidal space, constantly bathing the microvilli of hepatocytes at their vascular side.
- Kupffer cells: large branching cells derived from blood monocyte. Their pseudopodia are projected into the lumen of the hepatic sinusoids. Their cytoplasm shows many lysosomes and phagosomes containing hemosiderin pigment granules. The function of Kupffer cells: recognition and phagocytosis of aged RBCs with the digestion of their hemoglobin.
IV- The space of Disse
It is a narrow perisinusoidal space that exists between the endothelial lining of the sinusoids and the hepatocytes. It allows the exchange of metabolites between the plasma and the hepatocytes.
Contents of space of Disse
- Plasma filtered from the sinusoidal blood.
- Microvilli projecting from the hepatocytes.
- Reticular fibers forming a support to the wall of sinusoids.
- Hepatic stellate cells (Ito cells): they are vitamin A-storing mesenchymal cells.
Clinical hint: In chronic inflammation of the liver, hepatic stellate cells differentiate into myofibroblasts and deposit collagen type I in the perisinusoidal space causing liver fibrosis.
V- The biliary tree
The hepatocytes continuously synthesize and secrete bile that is poured into the bile canaliculi. These are lined by the cell membrane of adjacent hepatocytes. The bile canaliculi form a complex anastomosing network of channels that direct the bile towards the periphery of the hepatic lobules into the short canals of Hering lined by cuboidal cells.
Bile flows from the canals of Hering to end in the interlobular bile ducts in the portal canals. Bile ducts are lined by cuboidal then columnar epithelium. Bile ducts gradually enlarge and fuse forming the right and the left hepatic ducts.
Clinical hint: Experimental models on hepatic injury refer to the role of the cells lining the canals of Hering as hepatic stem cells capable of proliferation, differentiation, and liver regeneration.
VI- Hepatic lobulation
Three different classifications of liver lobules are described which refer to different aspects of hepatocyte activity, these are:
The classic hepatic lobule
It is a hexagonal mass of hepatocytes radiating around a central vein into which the sinusoids of this area drain. In the classic hepatic lobule, blood and bile flow in opposite directions; the blood flows towards the central vein whereas the bile flows away from the central vein. The portal canals are located at the corners of the lobule, formed of a small triangular area of connective tissue and enclosing the portal triad, containing:
- An interlobular bile duct.
- An interlobular branch of the portal vein.
- An interlobular branch of the hepatic artery.
The portal lobule
This is a triangular mass of hepatocytes from three adjacent classic hepatic lobules. It has at its center a portal canal and at each of its three angles a central vein. Each portal lobule drains its bile into the centrally-located bile duct.
The liver acinus
This is the functional unit of the liver. It is a diamond-shaped mass of hepatocytes from two adjacent classic hepatic lobules. It has a central vascular core formed of branches from the portal vein and hepatic artery lying along the border between two classic lobules. The liver acinus can be subdivided into three zones according to their blood supply:
- Zone I: the hepatocytes close to the vascular core. This zone is richly supplied by blood with excellent content of nutrients and oxygen. Hepatocytes of this zone carry out oxidative metabolism and protein synthesis.
- Zone II: hepatocytes intermediate in location and also in their blood supply.
- Zone III: the hepatocytes farthest from the blood supply, close to the central veins. This zone has the poorest blood supply almost exhausted of nutrients and oxygen. Hepatocytes of this zone carry out glycolysis and are the first hepatocytes that suffer from degeneration and necrosis.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Histology of pancreas, Structure of islets of Langerhans, Insulin function and Metabolism
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut and hindgut
Pancreas function, anatomy, parts, relations, ducts and blood supply