Pituitary gland function, structure, location, hormones and anatomy
The pituitary gland controls several other hormone glands in your body, including the thyroid & adrenals, the ovaries & testicles, so it is called the master gland, It is a protrusion off the bottom of the hypothalamus at the base of the brain, the pituitary gland is attached to the base of your brain by a thin stalk. It is about the size of a pea, It is situated in a bony hollow, just behind the bridge of your nose.
Anatomy of Pituitary gland
The pituitary gland is a small ovoid body that is lodged in the hypophyseal fossa (sella turcica) of the sphenoid bone. It is connected to the tuber cinereum of the brain by a hollow conical stalk called the infundibulum. It is roofed by the diaphragm sellae.
Relations of pituitary gland
- On each side: it is related to the cavernous sinus and its contents. It is related to the diaphragm sellae which separate the gland from the optic chiasma.
- Superiorly: It is related to the diaphragm sellae which separate the gland from the optic chiasma.
- Inferiorly: it is related to the body of sphenoid and sphenoid air sinus which separates the gland from the nasopharynx. It is separated from the floor of the hypophyseal fossa by the dura and the intercavernous sinus.
- Anteriorly: it is related to the tuberculum sellae and sphenoid air sinus which separates the gland from the cavity of the nose.
- Posteriorly: it is related to the dorsum sellae which separates the gland from the pons and the basilar artery.
- Arterial supply: It is supplied by superior and inferior hypophyseal arteries from the internal carotid arteries on each side.
- Venous drainage: It is drained by short veins into the surrounding dural sinuses.
Anatomical division of the pituitary gland
- Anterior lobe: it lies anterior to the hypophyseal cleft.
- Posterior lobe: it lies posterior to the hypophyseal cleft.
Histological organization of the pituitary gland
The pituitary gland is divided into:
- The anterior adenohypophysis.
- The posterior neurohypophysis.
Adenohypophysis
It is the darkly stained cellular part of the pituitary gland. It is subdivided into 3 parts:
1) Pars distalis
It is composed of branching cords of polygonal cells surrounded by sinusoidal capillaries and supported by a network of (reticular fibers. The cells are of two types:
i. Chromophobes (52%), which have a weak affinity to stains. Chromophobes are cells smaller than the chromophils and have agranular pale cytoplasm. By EM, the cell organelles are few in the cytoplasm. Function: chromophobes do not secrete hormones. They are considered as reserve cells or degranulated chromophils (have no granules).
ii. Chromophils (48%), which have a great affinity to stains. They have granular darkly stained cytoplasm which classifies them into two types:
- a) Acidophils: which have a great affinity to acidic stains. to basic stains.
- b) Basophils: which have great affinity.
a- Acidophils (37%)
They secrete hormones of a protein nature. When these cells are stained with periodic acid Schiff (PAS) reagent, which is a stain specific for glycoprotein molecules, they do not take the magenta-red color of the stain. They are said to be “PAS-ve”.
Generally, these cells are smaller than the basophils but contain larger secretory granules. Acidophils are of two types: somatotrophs & mammotrophs.
- Somatotrophs: secrete growth hormone.
- Mammotrophs (Lactotrophs): secrete prolactin hormone. The secretory granules in these cells are small but in pregnant and lactating females they become large and numerous. The cells in this case are called pregnancy cells or Erdheim cells. When sucking is terminated, lysosomes eliminate the excess secretory granules, a process known as crinophagy.
b. Basophils (11%)
They secrete hormones of glycoprotein nature so they and PAS +ve. Generally, they are larger than the acidophils, but contain smaller secretory granules. Basophils are of three types:
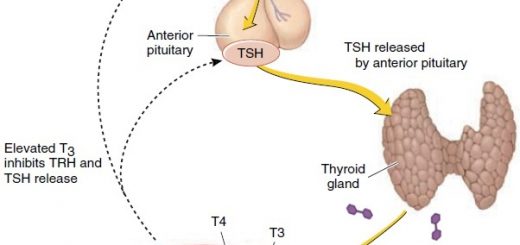
- Thyrotrophs secrete thyroid-stimulating hormone (TSH).
- Gonadotrophs secrete two hormones: Follicle-stimulating hormone (FSH), and Luteinizing hormone (LH).
- Corticotrophs: secrete an adreno-corticotrophic hormone (ACTH).
2) Pars tuberalis
It is the funnel-shaped superior extension that surrounds the infundibular stalk. It is highly vascular. It is formed of chromophobe-like cells. Function: non-specific.
3) Pars intermedia
It lies between the pars distalis and pars nervosa. In humans, it is a rudimentary region. In lower animals, it is made up of colloid-filled follicles which represent remnants of Rathke’s pouch. Function: non-specific.
Neurohypophysis
It lies posterior to the hypophyseal cleft. It is a pale stained fibrous part. It includes:
- The median eminence, which is a funnel-shaped downward extension of the hypothalamus.
- The Infundibular stalk, which together with the surrounding pars tuberalis constitutes the infundibulum.
- The pars nervosa, which is connected to the base of the brain by the infundibular stalk and the median eminence.
Pars nervosa
It consists of:
- Unmyelinated axons of neurosecretory cells are present in the supraoptic and paraventricular nuclei of the hypothalamus. These axons form the hypothalamo-hypophyseal tract, they carry the neurosecretion from the hypothalamic nuclei to the pare nervosa.
- Herring bodies: they are eosinophilic bodies that represent the accumulation of neurosecretory granules in axonal dilatations.
- Pituicytes: they are modified branched glial cells that have to supporting, isolation as well as nutritive functions.
- Rich fenestrated blood capillary plexus.
Development of pituitary gland
Origin:
- Buccal primordium from the roof of stomodium (somatic ectoderm) → Rathke’spouch → adenohypophysis.
- Cranial primordium from the floor of the diencephalon (neuro-ectoderm) → pars nervosa → neurohypophysis.
Development:
1- Buccal primordium:
- Rathke’s pouch → grows cranially → Rathke’s stalk → degenerates.
- The anterior wall of the pouch → thickened → pars distalis & the posterior wall → thinner → pars intermedia.
- Pars distalis → pars tuberalis.
2- Cranial primordium
- Pars nervosa grows caudally behind Rallike pouch. its stalk is called infundibulum.
- Pars nervosa will adhere pars intermedia → posterior lobe.
- Pars distalis + pars tuberalis → anterior lobe.
Congenital anomalies
- Craniopharyngeal canal: Due to failure of degeneration of the Rathke’s stalk→ communication between the nasopharynx and hypophyseal fossa → infection of the brain (fatal).
- Pharyngeal pituitary gland: Due to failure of ascend of buccal pituitary → present in the roof of nasopharynx may be removed during an adenoidectomy.
- Agenesis of the gland.
Hypothalamic-Hypophyseal Connections
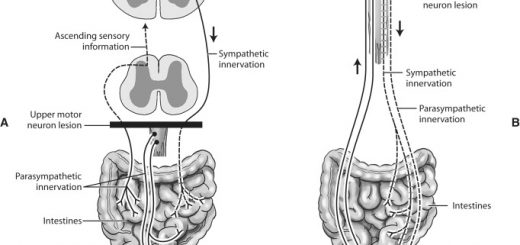
There are 2 types of connections between the hypothalamus and pituitary:
- A vascular connection between the hypothalamus and anterior pituitary gland in the form of a hypothalamic-hypophyseal portal circulation.
- A nervous connection between the hypothalamus and posterior pituitary gland in the form of the hypothalamic-hypophyseal tract.
Neurosecretion and neurohormones:
Neurohormones are hormones synthesized and secreted from special neurons into the circulation. Neurosecretion contains the following hormones:
1) – posterior pituitary hormones:
The posterior pituitary hormones are initially synthesized in the cell bodies of the supraoptic & paraventricular nuclei of the hypothalamus, and then transported in combination with “carrier” proteins called neurophysins down to the nerve ending in the posterior pituitary.
Stimulation of the hypothalamic nuclei initiates action: potentials in their neurons, transmitted downward along the fibers from the supraoptic or paraventricular nuclei on reaching the nerve endings, cause the release of hormone by the usual secretory mechanism of exocytosis and is absorbed into adjacent capillaries from which they reach the general circulation.
2). Hypothalamic releasing and inhibiting hormones
These hormones are synthesized in the hypothalamus and transported to the anterior pituitary through the hypothalamic-hypophyseal portal circulation.
Anterior pituitary gland function, hormones, location and Effects of Growth Hormone
Endocrine system structure, function, disorders, Endocrine Glands and Hormones types
Endocrine system, Endocrine glands, Pituitary gland and Hormonal coordination in living organisms
Posterior pituitary gland hormones & function, Control of ADH and Oxytocin hormone
Thyroid gland, Diseases of thyroid gland and Function of Parathyroid glands
Regulation of Growth Hormone Secretion and Effects of Deficiency of Anterior Pituitary Hormones