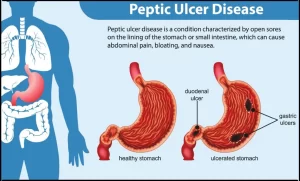
Peptic Ulcer Diseases symptoms, causes, what is the fastest way to cure a stomach ulcer?
Peptic ulcer disease (PUD) refers to open sores or ulcers that develop in the inner lining of the stomach, duodenum (first part of the small intestine), or, less commonly, the esophagus. These ulcers occur due to the corrosive effects of stomach acid and digestive enzymes.
Peptic Ulcer Disease (PUD)
- Hospital admission reduction by 43% in the USA.
- 50% reduction in Sweden.
- No drop for complicated D.U. Even increase in some studies.
- Now it is clear that there is an incidence of chronic asymptomatic ulceration of the stomach and duodenum.
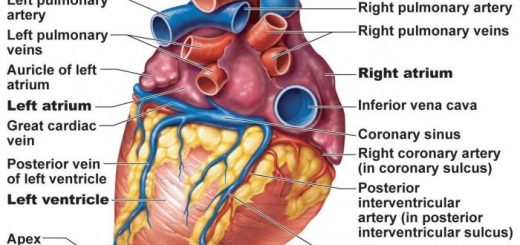
- Bleeding occurs in 20% of patients with DU. It may occur without a history of dyspepsia.
Bleeding Peptic Ulcer
- Continues or recurs in only 26% almost always within 2-3 days.
- Mortality is up to 37%.
- Overall mortality of bleeding ulcers is 6-7%.
- 20% of patients of D.U. as haematemesis or melena.
Upper GI bleeding in Egypt:
- Bleeding O.V., erosive gastritis, D.U., Ca. stomach, G.U.
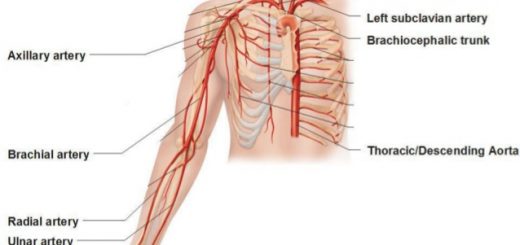
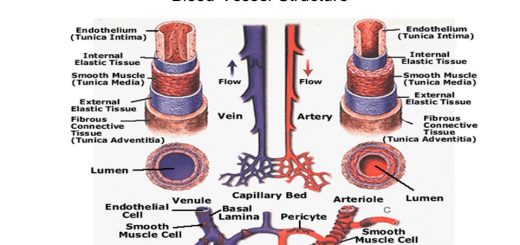
- Post ulcer erodes the gastroduodenal artery, ant. ulcer → no severe bleeding.
Presentation:
- Sudden massive haematemesis → Shock.
- Slow (usually melena)→ Ch. anemia.
Causes
The primary causes of PUD include:
- Helicobacter pylori (H. pylori) infection – A bacteria that weakens the stomach lining, making it more vulnerable to acid damage.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) – Medications like aspirin, ibuprofen, and naproxen can irritate the stomach lining and reduce protective mucus production.
- Excess stomach acid production – Conditions like Zollinger-Ellison syndrome can cause excessive acid secretion.
- Lifestyle factors – Smoking, alcohol consumption, stress, and spicy foods can worsen symptoms but are not direct causes.
Symptoms
- Burning or gnawing pain in the stomach (often worse on an empty stomach).
- Nausea or vomiting.
- Bloating and fullness.
- Loss of appetite and weight loss.
- Dark, tarry stools (a sign of bleeding ulcers).
- Vomiting blood (in severe cases).
Complications
If untreated, PUD can lead to:
- Bleeding ulcers – Internal bleeding that may cause anemia or hemorrhage.
- Perforation – A hole in the stomach or intestine leading to infection (peritonitis).
- Gastric obstruction – The scar tissue from ulcers can block food passage, causing vomiting and weight loss.
Diagnosis
- Endoscopy – A thin tube with a camera examines the stomach lining.
- H. pylori testing – Blood, stool, breath, or biopsy tests detect H. pylori infection.
- Barium swallow X-ray – Helps visualize ulcers.
- Typical history.
- Epigastric tenderness.
A. Site → posterior. B. Risk signs: (Forrest classification).
Forrest classification:
- Spurter.
- Visible vessel.
- Adherent clot.
- Red or black spot in the base of the ulcer.
Endoscopic Clues for Risk of Rebleeding:
- Visible vessel (blue or red). Protruding lesion with ulcer base, 50% rebleeding.
- Spurter (arterial).
Black or red spot. Overlying clot. 10% rebleeding
Treatment
Medications:
- Proton pump inhibitors (PPIs) – Omeprazole, lansoprazole, pantoprazole (reduce acid production).
- H2 receptor blockers – Ranitidine, famotidine (reduce acid secretion).
- Antacids – Neutralize stomach acid.
- Antibiotics – Treat H. pylori infection (e.g., clarithromycin, amoxicillin, metronidazole).
- Cytoprotective agents – Sucralfate, misoprostol (protect stomach lining).
Lifestyle modifications:
- Avoid NSAIDs and smoking.
- Reduce alcohol and caffeine intake.
- Manage stress and eat a balanced diet.
- Surgery (rare cases) – For severe ulcers with complications like bleeding or perforation.
D.U. Treatment:
- D.U. in contrast to G.U. should be regarded primarily as a medical disease that sometimes requires surgery. (80% will stop without intervention).
- Selection of operative treatment of the wrong patient who even hangs around the neck of his surgeon. He cannot eat or work with vomiting and pain.
- H2 blockers, proton pump inhibitors, somatostatin, and prostaglandins.
PPI
- Bolus or infusion, no difference.
- Better than H2 blockers (stronger and faster).
- Continue PPI 72 hours IV then oral.
- Combination of endoscopy and PPI.
Endoscopic treatment as mentioned above
Surgery:
Absolute Indications (in about 25%):
- Massive bleeding requiring >10 units.
- Rebleeding after cessation → Early surgery Death rate >30.
- Visible bleeding vessel on endoscopy →50% rebleeding.
Relative Indications:
- Giant G.U. or D.U.
- Visible vessel.
- Shortage of blood.
- Previous hemorrhage for the same lesion.
Lines
- The use of a definitive ulcer-curing operation is mandatory in patients with hemorrhage but optional in patients with perforation.
- Pyloromyotomy under run the vessel.
- PG or TV + GJ.
Recurrent bleeding in both → 13%
Mortality of PG is 8% double that of TV + gj.
Gastrectomy after all is a gastrectomy, the specimen is in the pot. But vagotomy may be complete or incomplete with no way of knowing except a one-week insulin test).
Fundamental Procedures:
Vagotomy
- Truncal vagotomy + Drainage (gastro jujonostomy-pyloroplasty).
- Selective vagotomy + Drainage.
- vagotomy+ Antrectomy (40%).
Partial gastrectomy (65-75%)
- The fact that 40-50% of patients are satisfied after vagotomy is attributable more to the reserve capacity of the stomach rather than the merits of the operation.
- Relative contraindications of surgery: youth, short ulcer history, atypical pain, heavy drinking, absence from work, and use of tranquilizers.
Rebleeding:
Most difficult to define
- Requirement of 7 units or more of blood over 48 hours period.
- or clinical evidence of further bleeding coupled with a 5 cm drop in CVP.
- Recurrence of haematemsis or bleeding in a nasogastric tube.
- Recurrence of melena or haematochezia coupled with unstable vital signs:
- Systolic < 90 mmHg. HR > 110 beats/min.
- Orthostatic drop of BP >20 mmHg or HR >20 beats/min.
- Decrease in hematocrit of > 4% in 24 hours.
Incidence: 5%
- Most patients re-bleed within 2 days from the time of the first episode.
- Re-bleeding carries a tenfold increase in mortality (MR=25%).
- So, if risk signs →active treatment.
- if rebleeding →surgery.
The rate of rebleeding:
- Endoscopic methods 20-25%.
- No endoscopic method 50-75%.
Endoscopic haemostasis:
- 60% reduction in rebleeding & need for surgery.
- 30% reduction in mortality.
Prognosis:
- Mortality of emergency operation 8-10%.
- Mortality of elective or semi-elective 1-2%.
Major prognostic information (endoscopic):
- Stigmata or recent hemorrhage (Forrest classification).
- Size of ulcer.
- Location of ulcer.
Clean Ulcer Base
- Most common in 50% of ulcer bleeds
- Rebleeding about 5%.
- Should not undergo endoscopic haemostasis.
- If rebleeding so either overlooked visible vessel or a second source of bleeding.
Non-bleeding Visible Vessel:
- Small raised protuberant or plug in the base of the ulcer.
- Found in less than 20% of ulcer bleed.
- About 40-50% rebleed without endoscopy.
- From translucent visible vessel→ 90% rebleeding.
- Red or purple→ 38%.
TAE Trans-arterial embolization if available then surgery.
You can subscribe to Science Online on YouTube from this link: Science Online
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion