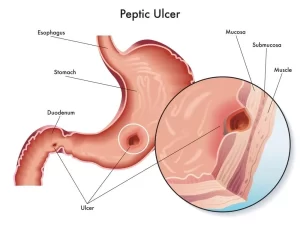
Peptic ulcer cause, types, symptoms, treatment and can a peptic ulcer be cured?
A peptic ulcer is an open sore in the stomach‘s inner lining or the duodenum (the first part of the small intestine) due to acid damage. You should avoid spicy foods, caffeine, and alcohol, quit smoking, reduce NSAID use (switch to acetaminophen if possible), eat smaller, frequent meals, and manage stress.
Peptic ulcer
An ulcer occurs due to erosion of the Gl mucosa resulting from the digestive action of HCL and pepsin.
Sites:
- Duodenum (commonest).
- Stomach.
- Jejunum after gastro-jejunostomy.
- Lower oesophagus due to reflux oesophagitis.
- Meckel’s diverticulum (rarest).
Etiology: imbalance between aggressive and defensive factors:
Aggressive factors:
- HCL stimulation (nervous by the vagus nerve, mechanical and hormonal).
- HCL is secreted by parietal cells and has a PH of 0.8.
- PH reaches 2:3 after mixing with food at which pepsinogen is activated to pepsin.
- Ulcerogenic drugs: inhibit the synthesis of protective PG (NSAIDS, corticosteroids, erythromycin, methotrexate, cyclophosphamide, azathioprine, Iron, kcl).
Protective factors: mucus secreted by goblet cell, blood supply, PG.
Types of Peptic Ulcers
- Gastric Ulcer – Forms in the stomach.
- Duodenal Ulcer – Forms in the duodenum (more common than gastric ulcers).
Causes of Peptic Ulcers
- Helicobacter pylori (H. pylori) infection – A bacteria that weakens the stomach lining.
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) – Long-term use of aspirin, ibuprofen, or naproxen can damage the stomach lining.
- Excess stomach acid production – Caused by stress, spicy foods, or Zollinger-Ellison syndrome (rare).
- Smoking and Alcohol – Irritate the stomach lining and increase acid production.
- Stress and Diet – Do not directly cause ulcers but can worsen symptoms.
Symptoms of Peptic Ulcers
- Burning stomach pain (worse on an empty stomach, relieved by food or antacids).
- Bloating, nausea, or vomiting.
- Loss of appetite or unexplained weight loss.
- Dark or tarry stools (bleeding ulcer) – Requires urgent medical attention.
Diagnosis
- Endoscopy – A camera is inserted into the stomach to check for ulcers.
- H. pylori test – Breath, stool, or blood test.
- Barium X-ray – Used in some cases to see the digestive tract.
Treatment of Peptic Ulcers
Medications:
- PPIs (Proton Pump Inhibitors) – Omeprazole, Pantoprazole (reduce stomach acid).
- H2 blockers – Ranitidine, Famotidine (less commonly used now).
- Antibiotics – If H. pylori is present (combination therapy).
- Antacids – Provide temporary symptom relief.
- Cytoprotective agents – Sucralfate, Misoprostol (protect stomach lining).
Lifestyle Changes:
- Avoid spicy foods, caffeine, and alcohol.
- Quit smoking.
- Reduce NSAID use (switch to acetaminophen if possible).
- Eat smaller, frequent meals.
- Manage stress.
Surgery (Rare Cases):
If ulcers bleed, perforate, or don’t heal with medication.
Diagnostic studies
Endoscopy (size, shape, site) is most often used.
- tissue biopsy to identify H.pylori and to rule out gastric cancer.
- Follow-up: determines the degree of ulcer healing after treatment.
Medical treatment
- proton pump inhibitors (decrease HCL secretion by inhibiting parietal cell H/K ATP pump).
- H2-blockers (selectively block H2 on parietal cells, treatment duration is 6-8 weeks) used in the past.
- sucralfate (binds proteins in exudates and forms viscous adhesive that protects gastric mucosa) used in the past.
Surgery for uncomplicated PU in the past, is now obsolete after the invention of PPI.
PUD complication
- major complications (hemorrhage, perforation, gastric outlet obstruction) Others
- (intractability, malignancy, hour glass stomach, recurrence of ulceration).
1. Hemorrhage (upper GI bleeding)
The 2nd most common cause of UGI bleeding after the varices. (44% of all upper gastrointestinal (GI) hemorrhage). Usually With posteriorly located DU within 2cm from the pylorus (because of gastroduodenal artery) which Develops from erosion of:
- granulation tissue at the base of the ulcer.
- erosion of blood vessels mainly a branch of gastroduodenal artery.
One-third of patients with peptic ulcer (PU) hemorrhage have no previous history or diagnosis of PU disease. Hemorrhage is the leading cause of death due to PU disease with 5-10%.
Clinical picture:
- melena: black offensive tarry stool.
- Haematemsis, coffee ground (in small amounts).
- Hypovolemic shock.
- Acute anemia.
- rarely, in severe bleeding, bleeding per rectum.
Initial management (Resuscitation)
- assess shock and replace blood loss (pulse, BP, urine output, haematocrit).
- stop bleeding by ice-water lavage) through NGT.
- history and physical examination.
- upper Gl endoscopy (within 1-2 hours of admission).
- Although spontaneous cessation of bleeding occurs in 70% of patients, endoscopy is still indicated as the first-line investigation in order to identify and often treat the bleeding point. It should be performed within 24 hours of the initial presentation, especially in patients with hypotension, age older than 60 years, and multiple co-morbidities.
Lines of management
1. medical treatment (intravenous fluid, antibiotics, anticoagulants, blood transfusion after loss of 30% of circulating blood volume, PPIs). In conjunction with endoscopic therapy, pharmacological therapy is started:
- Acid suppression by proton-pump inhibitors (PPIs) maintains intra-gastric pH > 6 to stabilize clots and prevent rebleeding. (Omeprazole 80 mg bolus injection is administered followed by 8 mg/hour intravenous (IV) infusion for 72 hours.
- Tranexamic acid.
- Eradication H-pylori infection.
2. Endoscopic treatment (persistent ulcer)
3. surgical treatment (in case of failure of endoscopic failure and when requiring a large amount of blood transfusion).
4. interventional radiology: embolization patients, patients unfit for anesthesia/surgery.
Endoscopic treatment
In the presence of major signs of recent hemorrhage, endoscopic therapy significantly reduces the risk of re-bleeding. Methods include the following:
- Injection: 1. Adrenaline: typically, a 0.5-1 ml of diluted. adrenaline (1:100000) into each of the four quadrants of the ulcer base. 2. Ethanol. 3. Variceal sclerosants (sclerosing agents).
- cautery by heat probe or electrocautery.
- YAG laser.
- Hemoclips.
Surgery
- Surgery is indicated when there’s active hemorrhage refractory to endoscopic techniques
- patients who require more than 6 units of blood require surgery.
- Rebleeding in hospital.
Duodenal ulcer:
- exploration.
- Mobilization (kocherization).
- duodenotomy: transverse
- under running/triple stitch sutures of the bleeding point
- ligation of GDA.
- Truncal vagotomy.
- Closure
In case of bleeding gastric ulcer
- Antrectomy and gastro-jejunostomy) to prevent re-bleeding and exclude malignancy.
- exploration.
- excision of ulcer by distal gastrectomy or wedge resection.
- Take biopsy.
- Closure.
2- perforation
- occurs when the ulcer penetrates the serosal surface with spillage of contents into the peritoneal cavity → peritonitis (2 stages).
- usually related to non-steroidal anti-inflammatory drug (NSAID) intake.
- Anteriorly situated ulcers perforate more readily.
- More common with duodenal ulcers.
- More common in males than females.
- 50% of patients have no history of peptic ulcer disease.
- Stage of chemical peritonitis: the peritoneum will react by production of alkaline fluid neutralizing the acidity → peritonitis which is sterile) so-called Chemical Peritonitis. This stage lasts for 12 hours).
General: normal but still tachycardia,
Local:
- Inspection: no abdominal movement with respiration.
- Palpation: tenderness (maximum at epigastrium), board abdomen, and rebound tenderness.
- Percussion: Obliterated liver dullness due to escape of gas from perforated gut under diaphragm & shifting dullness) due to the escape of free bile in the peritoneum.
Stage of septic peritonitis: classic peritonitis
toxic symptoms → septic shock.
General: patient is toxic (FHMA).
Local: silent distended abdomen on auscultation.
Notes:
- Moynhan ‘s sign) Perforation with pain in right iliac fossa→ Fluid may track along the right paracolic gutter to the right iliac fossa causing pain in the right iliac fossa.
- sealed perforation: intestine and omentum come and bulge this perforation so the patient’s condition improves → conservative treatment without surgery.
- acute abdomen: pain –distress-shallow breath-rigidity (peritonitis)-absent gut sounds and tympanitic notes over the liver.
Differential diagnosis
- Pancreatitis.
- Gastric.
- acute cholecystitis.
- ruptured aortic aneurysm.
- Angina, MIL.
- pneumonia
Laboratory investigations
- CBC: Leucocytosis.
- raised serum amylase.
Imaging
- Plain x-ray abdomen: standing with visualization of diaphragm shows gas under right copula of diaphragm→
- Us: fluid collection due to its escape from the perforation.
- Plain CT: massive pneumoperitoneum.
Treatment option
- Medical: in case of sealed perforation.
- Endoscopic contraindicated Interventional.
- radiology: limited role.
- The main treatment is surgery.
Preoperative preparation:
- Nothing per mouth.
- Monitoring urine output.
- Nasogastric (NG) tube.
- Analgesia e.g. opioids.
- Proton pump inhibitors (PPIs).
- Vigorous fluid resuscitation.
- Correction of electrolyte imbalance.
- Broad-spectrum Antibiotics.
- Central venous pressure (CVP) measurement.
Surgical Treatment of Perforated Duodenal Ulcer
- Laparotomy: Midline exploratory incision.
- Peritoneal lavage/toilets to remove all toxic fluid and food debris.
- Omental (Graham) patch to reinforce the approximated edges of the ulcer.
- The operation can be performed laparoscopically.
Surgical Treatment of Perforated (Gastric Ulcer)
- Options include the following:
- Simple closure.
- Wedge resection.
- Biopsy.
- Antrectomy and gastro-jejunostomy.
3- Gastric outlet obstruction
- Pyloric stenosis is a misnomer as the obstruction is distal to the pylorus.
- usually, a long history of ulcer pain.
- obstruction is not totally due to fibrous scar tissue (severe cases) also there is edema, inflammation, and spasm.
- Short duration or absence of pain increases the possibility of malignant obstruction.
Clinical manifestation
- Vomiting: nonbilous, old food, bad odor.
- May show swelling of the upper abdomen of a distended stomach.
- Visible peristalsis.
- Dehydration due to malabsorption.
- tetany due to relative hypocalcemia.
- constipation.
- succession splash.
- loss of weight.
- Epigastric pain.
Laboratory investigations show:
- anemia.
- metabolic (hypochloremic) alkalosis.
- hyponatremia (Na lost in urine with HCO3).
- hypokalemia as k lost in the urine with H (after Na retention) acidic urine.
- hypocalcemia (due to alkalosis as it decreases ionized Ca).
- elevated urea and creatinine levels.
Endoscopy
- the pyloric opening is deformed and narrow.
- You must take a biopsy to exclude malignancy.
Imaging:
- Barium meal: soap dish appearance indicating very distended stomach.
- CT with IV contrast: intestine is collapsed.
Treatment aim
- correction of metabolic abnormalities (Iv saline with k).
- dealing with the mechanical problem.
- correction of anemia (blood transfusion).
- Gastric lavage and suction (5-7 days) by NG tube.
Treatment options
- Medical: in mild cases (Iv PPI).
- Endoscopic: patients unfit for surgery/anesthesia (Balloon dilatation or stent).
- Surgery’s main role.
- Interventional radiology: No role.
Note:
- In mild cases, inflammation and partial obstruction may resolve with gastric lavage, acid suppression therapy and antispasmodics.
- In severe cases, a hard-fibrotic stricture develops causing a dilated atonic stomach.
Surgical treatment:
Pre-operative Preparation:
- Correction of fluid and electrolyte abnormalities by normal saline and potassium.
- Nasogastric lavage.
- Proton pump inhibitors.
Truncal vagotomy with drainage procedures such as gastrojejunostomy or pyloroplasty.
Truncal vagotomy denervates the antropyloric mechanism SO, another procedure is needed to bypass the pylorus which is: [Gastrojejunostomy)
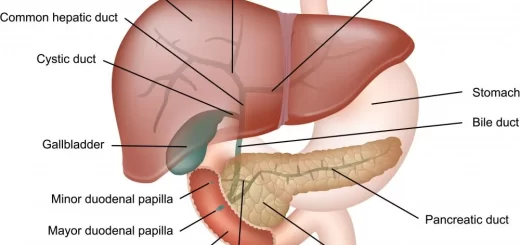
Zollinger-Ellison syndrome (Gastrinoma):
Is a disease in which tumors cause the stomach to produce too much acid resulting in peptic ulcers.
- 0.1 to 1 percent of patients with peptic ulcer disease.
- Symptoms are similar to a typical ulcer.
- Symptoms may be controlled by standard doses of an antisecretory drug.
- Patients may not be tested for hyper gastrinemia.
- Gastrinoma can be either sporadic (80%) or associated with MEN TYPE 1.
Tumour location
- gastrinoma triangle 80%.
- pancreas 50-60%.
- duodenum 40-50%.
- 20-25% related to MEN-1.
- 50-70% malignant lymph node.
symptoms
Gastritis – recurrent ulcer – diarrhea (malabsorption).
signs of ZES
- multiple ulcers.
- Ulcer in atypical site.
- Diarrhea.
- severe esophagitis.
- Resistant ulcer.
- enlarged gastric folds.
Treatment:
- Surgical: if not metastatic.
- Chemotherapy: If metastatic.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion