Parathyroid gland anatomy, structure, function, hormones and Tetany types
Parathyroid glands regulate the calcium levels in our bodies, they are located behind the thyroid at the bottom of your neck, they are about the size of a grain of rice, they produce and secrete parathyroid hormone in response to low blood calcium, which plays an important role in regulating calcium in the blood & within the bones, Calcium is the most important element in our bodies, so calcium is regulated than any other element with the parathyroid glands.
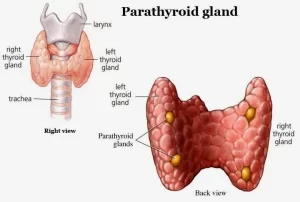
Anatomy of Parathyroid gland
They are four small, oval, yellowish-brown bodies that usually lie between the posterior lobar borders of the thyroid gland and its capsule; there are two glands on each side, superior and inferior one, the upper parathyroid glands are usually found adjacent to the posterior surface of the middle part of the thyroid lobe. The lower parathyroid glands are found on the lateral or posterior surface of the lower part of the thyroid lobe (their position is variable).
Arterial supply: inferior thyroid artery
Nerve supply: Sympathetic fibers are distributed from the superior and middle cervical ganglia of the sympathetic trunk. These fibers are not secretory to the gland because the parathyroid activity is controlled by the level of the blood calcium.
Histological structure of the Parathyroid gland
Stroma
The thin CT capsule sends septa inside the gland, from which reticular fibers arise forming a network supporting the parenchymal cells, A rich network of fenestrated blood capillaries surrounds the cells.
Parenchyma
It is formed of densely-packed cords of cells of two types, these are:
A. The chief cells:
- By LM: They are small polygonal cells with large euchromaticnuclei and pale cytoplasm. These cells are numerous.
- By EM: The cytoplasm contains a moderate amount of organelles of polypeptide secreting cells with secretory granules. Glycogen granules and lipid droplets are also present and they are the cause of the pale cytoplasm seen with the LM.
- Function: secretion of parathyroid hormone (PTH).
B. Oxyphil cells:
By LM:
- They are few in number, usually found in clusters.
- They are large polygonal cells with small dense nuclei and deep eosinophilic cytoplasm.
By EM: The cytoplasm contains many mitochondria with abundant cristae which are the cause of eosinophilia observed by LM.
Function: unknown
With increasing age:
- The chief cells are replaced by fat cells (adipocytes). The adipocytes may constitute more than 50% of the gland in old individuals.
- The number of oxyphil cells increases.
Parathyroid hormone (parathyrin)
Parathormone (parathyroid hormone) is composed of 84 amino acid residues. It is synthesized as a 115 amino acid precursor molecule pro-PTH.
Mechanism of action of parathormone
Parathormone binds to a membrane receptor protein which appears to be identical in bone and kidney but found in non-target organs.
The hormone-receptor interaction initiates a typical cascade: activation of adenylatecyclace → increased intracellular cAMP → activation and phosphorylation of intracellular enzymes → mediates biological action.
Actions of parathyroid hormone (PTH)
The effect of parathormone is the elevation of calcium ion concentration in the extracellular fluid and depression of phosphate concentration, so as to keep the solubility product constant (Ca x PO4 = constant). The parathormone produces its effects by the following actions on bones, gastrointestinal tract, and kidneys:
A) Effect on bones
It acts directly on the bone. It increases bone resorption and mobilization of calcium and phosphate to the blood. Such action occurs in two phases namely the rapid phase and slow phase:
- Rapid phase: It occurs within minutes after the release of PTH from the parathyroid gland, It results from the activation of the already existing osteoclasts.
- Slow phase: It requires days or even weeks to become fully developed. It results from the proliferation of the osteoclasts.
B) Effect on the intestine
It enhances both calcium and phosphates absorption from the intestine indirectly by increasing the formation of 1.25 dihydroxycholecalciferol (1,25 DHCC) from vitamin D. PTH increases the activity of the 1α hydroxylase enzyme in the kidney.
C) Effect on kidneys
- PTH increases calcium reabsorption from the distal convoluted tubules and collecting ducts.
- PTH increases the excretion of phosphate in urine (Phosphatiuric action) by decreasing phosphate reabsorption in the proximal convoluted tubules.
Regulation of parathormone secretion
1) Calcium ion concentration in the blood is the main factor for regulating the secretion of PTH in a negative feedback mechanism:
a) When plasma calcium is low, the secretion of PTH is increased within minutes, and if the decreased concentration persists, the glands will the (hypertrophy e.g. rickets, pregnancy, and lactation.
b) Any condition that increases the calcium ion concentration leads to decreased activity and reduced sizes of parathyroid glands such as:
- An excessive amount of calcium in the diet.
- Increased vitamin D in the diet.
- Bone resorption is caused by factors other than parathyroid hormone.
2) Phosphate concentration: When phosphate concentration increases, it stimulates PTH secretion.
Effects of hyposecretion of PTH (hypoparathyroidism)
Hypoparathyroidism will lead to:
- Decrease bone resorption.
- Increase Ca++ excretion in urine.
- Decrease intestinal absorption of Ca++.
- Decrease Ca++ level in plasma (hypocalcemia).
Effects of hypocalcemia
When the extracellular fluid concentration of calcium ions falls below normal (8.5-10.5 mg/dl), the nervous system becomes more excitable because of increased neuronal membrane permeability to sodium ions. This increase in excitability occurs both in the central nervous system and in the peripheral nerves (including neuromuscular junction).
The nerve fibers become so excitable that they begin to discharge spontaneously, initiating nerve impulses that pass to the skeletal muscles causing spastic contraction Tetany).
Tetany
It is a state of spastic contraction of skeletal muscles caused by increased neuromuscular excitability as a result of decreased calcium levels in the extracellular fluid below normal.
Causes of Tetany
- Hypoparathyroidism.
- Akalonis.
- Vitamin D deficiency.
- Low calcium content in the diet.
- Real failure (rarely).
Types and manifestations of Tetany
I- Manifest Tetany
It occurs if the plasma calcium level falls below 7 mg %. It occurs spontaneously during rest producing spastic contraction involving specially the muscles of extremities (carpo-pedal spasm), generalized convulsions may occur. In severe hypocalcaemia, tetany occurs so quickly that a person dies due to the contraction of some important muscles such as the laryngeal muscles leading to laryngeal stridor and death.
Il- Latent tetany
The plasma calcium level is about 7 mg % (7-9 mg %). This type of tetany does not occur spontaneously but it needs certain tests to provoke it:
- Chvostek’s sign: Tapping on the angle of the jaw stimulates the facial nerve and causes quick contraction of ipsilateral facial muscles.
- Trousseau’s sign: Occlusion of the circulation by tying a blood pressure cuff around the arm and arresting blood supply to the hand, cause carpal spasm (flexion at the elbow, wrist joints and metacarpophalangeal joints and extension of fingers and adduction of thumb).
Effects of hypersecretion of PTH (hyperparathyroidism):
Hyperparathyroidism will lead to:
- Increase bone resorption.
- Increase Ca++ reabsorption from renal tubules.
- Increase intestinal absorption of Ca++.
- Increase Ca++ level in plasma (hypercalcemia).
Effects on Bone
In severe hyperparathyroidism, the bone resorption is markedly increased, so the bone is decalcified. Multiple fractures can result from slight trauma. Radiographs of the bone show that the bone may be eaten away and filled with multiple cysts (Ostitis fibrosa cystica).
Effects of hypercalcemia
- Depression of the central and peripheral nervous system.
- Muscular weakness.
- Constipation, abdominal pain, and loss of appetite because of depressed contractility of the muscle wall of the gastrointestinal tract.
- Depressed relaxation of the heat during diastole.
- If the calcium level in plasma rises to a very high level, calcium phosphate crystals may be deposited in many tissues (metastatic calcification) e.g the alveoli of the lung, thyroid gland, tubules of the kidney (renal stone may be formed), and in the walls of arteries, this effect can be fatal.
You can follow Science Online on YouTube from this link: Science online
Regulation of Thyroid hormones secretion, Effects of Hyperthyroidism and Hypothyroidism
Histological structure of thyroid gland and Functions of Thyroid Hormones (T3 and T4)
Thyroid gland function, hormones, function, anatomy and Congenital anomalies
Posterior pituitary gland hormones & function, Control of ADH and Oxytocin hormone
Endocrine system structure, function, disorders, Endocrine Glands and Hormones types