Oxygen transport by blood, Importance of P50, Bohr Effect and Treatment of CO poisoning
Carbon dioxide gas diffuses out of the blood and into the alveoli to be expelled from the body, Oxygen gas diffuses across the alveoli, it enters the bloodstream, and is transported to the tissues where it is unloaded, However gas exchange is a continuous process, the oxygen & carbon dioxide are transported by different mechanisms.
Oxygen Transport
Oxygen can move from one point to another by diffusion due to the pressure difference from high pressure to low pressure.
Diffusion of O₂ (O₂-cascade)
PO₂ in dry atmospheric air is 159 mm Hg. Once this air enters the respiratory passages it is humidified with water vapour, PO₂ drops to 150 mm Hg. Alveolar PO₂ is 100 mm Hg. In pulmonary capillaries, PO₂ is 100 mm Hg while in systemic capillaries it drops to 95 mm Hg (due to physiological shunts).
When blood reaches the peripheral tissues, its PO₂ in the arterial side of capillaries is still 95mm Hg. The PO₂ in the interstitial fluid that surrounds the tissue cells is about 40mm Hg, Oxygen diffuses rapidly from the blood to the interstitial fluid (due to pressure difference) until pressure is equalized.
Therefore, in venous blood PO₂ equals 40 mm Hg. O₂ is always used by the cells therefore the intracellular PO₂ remains lower than Po2 in capillaries, It ranges between 5 and 40 mm Hg (average about 23 mm Hg) depending on the activity of the cell. The drop in PO₂ during its transport from the atmosphere to peripheral tissue cells is called O₂-cascade.
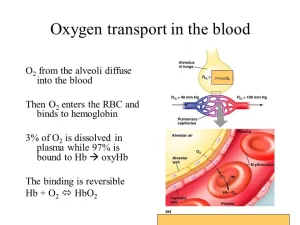
O₂ transport by Blood
O₂ is transported from the lungs to the tissues in 2 forms:
I- In physical solution (dissolved O₂)
About 3% of total O₂ in the blood. In arterial blood: 0.3 ml /100ml blood. It causes PaO₂ = 100 mm Hg. In venous blood: 0.13 ml/100ml blood. It causes PvO₂ = 40 mm Hg.
The amount of dissolved O₂ in the whole arterial blood which equals 5 liters (cardiac output) = 5000 x 0.3/100 =15 ml. This small amount is very important because it is responsible for O₂ tension or partial pressure in the blood which in turn determines.
- Direction and rate of flow of O₂.
- Amount of O₂ in chemical combination with Hb.
II- Oxygen in chemical combination
About 97% of O₂ is bound to Hb of RBC in chemical combination. Normally it is about 20 ml O₂ /dI of arterial blood. It is essential for supplying adequate O₂ to the tissues during rest and exercise.
O₂ content of the blood
It is the amount of O₂ present in 100 ml of blood in chemical combination with Hb. It depends on Hb concentration and O₂ tension. It is decreased in anemia (decreased Hb concentration) and hypoxemic hypoxia (decreased Po2 in arterial blood).
O₂ carrying capacity of the blood
It is the maximal amount of O₂ present in 100 ml of blood in chemical combination with Hb, when hemoglobin is fully saturated with O₂. One gram Hb can be combined with 1.34 ml O₂, The total amount of Hb in the blood is about 15 g/dl. Then, the amount of O₂ combined in 100ml blood when Hb is fully saturated equals 15 x 1.34 = 20ml/100ml.
Percentage of saturation of Hb with O2
The % saturation with O₂ is calculated as follows: (O₂ content/O₂ capacity) x 100
The proportion of Hb combined with O₂ depends on PO₂ irrespective of the amount of Hb present. At PO₂ 100 mm Hg the percentage saturation of Hb is 100%.
Oxygen pressure and content relations
- The relation between O₂ pressure and O₂ in physical solution is a linear relationship i.e. any increase in O₂ in physical solution leads to an increase in O₂ pressure.
- The relation between oxygen pressure and the % saturation of Hb with O₂ is not linear, it is S-shaped or sigmoid in nature. This is explained by O₂-Hb dissociation curve.
O₂-Hb dissociation curve
This curve shows the relation between PO₂ (tension) and the % saturation of Hb with O₂. The values are obtained by placing small volumes of blood in several glass containers called tonometers. Each one is exposed to a particular O₂ pressure at 37°C.
Enough time is allowed for equilibration, and then the blood is analyzed to determine its O₂ content. The % of Hb saturation with O₂ is calculated and plotted against the O₂ pressure. Oxygen Hb-dissociation curve has a characteristic sigmoid or S-shaped. This is due to a combination of oxygen with heam groups of Hb molecules.
Physiological analysis of the curve
1. The flat upper part represents a zone of Hb saturation with O₂. It occurs when O₂ tension or pressure is between 100-60 mm Hg. This is called the loading zone or association zone; where the affinity of Hb to combine with O₂ is high. It represents the lung side. Changes in PO₂ within the range of 100-60mm Hg. have little effect on % saturation of Hb with O₂. It drops from 100% to 90% In systemic arterial blood % saturation of Hb with O₂ is about 97.5% and O₂ content is about 19.4 ml /dl (PO₂ = 95 mm Hg due to physiological shunts).
2. The steep lower part of the curve occurs when O₂ tension decreases below 60mm Hg, the % saturation of Hb with O₂ decreases rapidly (low affinity). It is called the unloading zone or dissociation zone and represents the tissue side.
- At PO₂ 40 mm Hg (Tissues in resting condition), the % saturation of Hb is 75% and O₂ content is 14.4 ml /dl. About 25% of O₂ is given rapidly to the tissues when the pressure decreases from 95 to 40 mm Hg. It equals 5ml O₂/dl (19.4-14.4 = 5 ml O₂/dl) or (250 ml/min in the whole blood).
- At PO₂ 20mm Hg (during muscular exercise) Hb% saturation becomes 35% and O₂ content 6 ml /100 ml i.e. the blood gives the majority of its O₂ to the tissues.
P50 is the value of oxygen pressure at which the Hb is 50% saturated with O₂. It equals 26.5 mm Hg when % saturation is 50%, O₂ content = 10.1ml, temperature = 37°C, and pH 7.4.
Importance of P50
It determines the position of the O₂ dissociation curve, whether normal, shifted to the right, or to the left.
- If P50 is decreased: Hb affinity to O₂ is high, there is a shift of the curve to the left and less O₂ is delivered to the tissues.
- If P50 is increased: Hb affinity to O₂ is low which means a shift of the curve to the right, and more O₂ is delivered to the tissues.
The P50 is increased during exercise, because the temperature rises in active tissues and CO₂ and metabolites accumulate, lowering the pH. In addition, much more O₂ is removed from each unit of blood flowing through active tissues because the tissues PO₂ declines.
Bohr Effect
It is the CO₂-induced shift of the hemoglobin dissociation curve which is mainly due to the effect of CO₂ on pH. Thus the addition of CO₂ (at tissue level) causes a rightward shift of the hemoglobin dissociation curve increasing O₂ release, and the removal of CO₂ in the lung causes a leftward shift that promotes extra O₂ uptake by the blood.
2-3 Diphosphoglycerate
In anaerobic glycolysis, RBCS produce 2-3 DPG in high concentration. It binds to the β-chain of deoxygenated hemoglobin causing the release of O₂ from Hb.
Therefore, when 2-3 DPG increases in the RBC, the affinity of Hb to O₂ decreases, and the O₂-Hb dissociation curve is shifted to the right. On the other hand, when it decreases, the affinity of Hb to O₂ increases, and O₂– Hb dissociation curve is shifted to the left.
HbO₂ + 2-3 DPG ↔ Hb-2-3DPG + O₂
Factors that increase 2-3 DPG synthesis
- Chronic hypoxia (lung diseases).
- High altitude (PO₂ is low).
- Hormones as: thyroid hormones, growth hormone, and androgens.
- During muscular exercise 2-3 DPG formation is increased within one hour (especially in non-athletes).
- Anemia.
Other forms of Hb and their reactions
1. Fetal Hemoglobin (HbF)
It has a high affinity to O₂ and this facilitates O₂ transfer from the mother to the fetus. Fetal Hb has 2-Y polypeptide chains in place of the chains. 2-3 DPG combines only with the B-chain of deoxygenated Hb. Since this chain is absent in HbF, 2-3DPG does not bind with HbF.
This leads to an increase in HbF affinity to O₂ i.e. shifts the O₂-Hb dissociation curve to the left. This is beneficial to the fetus, as it facilitates O₂ transfer from the mother to the fetus Le. at any pressure of O₂, HbF would contain more O₂ than adult Hb.
2. Myoglobin
It is an iron-containing pigment found in skeletal muscle. It binds only one oxygen molecule rather than 4. Its dissociation curve is to the left of O₂-Hb dissociation curve. Its curve is in the form of a rectangular hyperbola rather than a sigmoid. This shape indicates that it readily takes up O₂ from Hb. It releases O₂ only at a very low PO₂.
The PO₂ in exercising muscle is close to zero. The myoglobin content is greatest in muscles specialized for sustained contraction. The muscle blood supply is compressed during such contractions, and myoglobin may provide O₂ when blood flow is cut off. When the muscle relaxes and the blood flow is re-established, myoglobin is recharged with O₂. 2-3 OPG does not influence myoglobin affinity to O₂.
3. Carboxyhemoglobin (HbCO)
Carbon monoxide is a toxic gas produced by incomplete combustion of carbon (fires, exhausts, neon illuminating gases, tobacco). It has (200-250) times greater affinity to Hb than does O₂. It interferes with the O₂ transport function of the blood. The addition of 0.1 % Co to air leads to 50% HbO₂ and 50% HbCO formation. CO lowers oxygen content without altering PaO₂.
HbCO is cherry red in color; it is visible in the skin, nail beds, and mucous membranes. The patient poisoned by CO looks pink and healthy. CO competes with O₂ for the same binding sites of Hb and, therefore can displace O₂ from the hemoglobin. All the binding sites that are bound to CO, do not respond to falling PO₂.
The remaining O₂ molecules on the Hb are much more strongly bound and unload slower than normal i.e. shift the curve to the left. Heavy cigarette smokers may have up to 14% of their Hb in the form of HbCO. Death results when about 70-80% of the circulating hemoglobin is converted to COHD.
Symptoms produced by chronic exposure to sublethal concentrations of CO are those of hypoxia and progressive brain damage, including mental changes and, sometimes, a parkinsonism-like state.
Treatment of CO poisoning consists of
- Immediate termination of the exposure.
- Hyperbaric oxygenation is useful in this condition. Exposure to 100% O₂ at 2 to 3 atmospheres (i.e. under high pressure) can increase dissolved O₂ in arterial blood to the point that arterial O₂ tension is greater than 2000 mm Hg and tissue O₂ tension is 400 mm Hg. If exposure is limited to 5 h or less at these pressures, O₂ toxicity is not a problem.
- Partial or complete blood exchange.
You can follow Science Online on YouTube from this link: Science online
Ventilation-perfusion relationships and why is ventilation higher at the base of the lung
Regional difference in ventilation, Pulmonary circulation, Shunt and Lung perfusion zones
Mechanics of ventilation, Structures of Respiratory system and Functions of conducting zone
Mechanics of Pulmonary Ventilation and Pressure changes during Respiratory cycle
Carbon dioxide transport from tissues to lungs, Tidal CO2 and Haldane effect