Ovary function, location, anatomy, structure, Oogenesis and maturation of primary oocyte
Ovaries are the female gonads, they secrete hormones, they protect the eggs a female is born with and they release eggs for possible fertilization, The ovary is located within a depression, the ovarian fossa, on the lateral pelvic wall at the level of the anterior superior iliac spine.
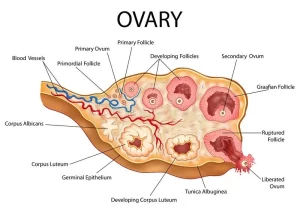
The ovary
The ovary is about the size and shape of an almond (3 length x 2 width x 1 thickness cm), it presents 2 surfaces: medial and lateral. Lateral surface: related to the peritoneum of the lateral pelvic wall and obturator nerves and vessels.
- Medial surface: covered with fimbriated end of the uterine tube.
- 2 Borders: Anterior and posterior
- Attached border: attached to the mesovarium.
- Free border: is free.
- 2 ends: tubal (upper) and uterine (lower):
- Tubal end; attached to fimbria and suspensory ligament of the ovary.
- Uterine end: is attached to the lateral angle of the uterus by the ligament of the ovary.
Ligaments of the ovary
- Suspensory ligament: It connects upper end of the ovary to the lateral pelvic wall and contains the ovarian vessels and nerves.
- Ovarian ligament: It connects the uterine end of the ovary to the lateral angle of the uterus.
- Mesovarium: It connects the anterior border of the ovary to the upper layer of the broad ligament.
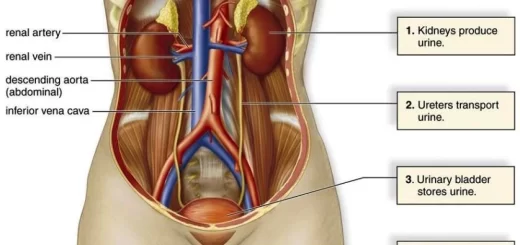
Arterial supply
Ovarian arteries: It runs through the suspensory ligament and then through mesovarian to reach the ovary.
Venous drainage
- Pampiniform venous plexus → Ovarian vein.
- The right ovarian vein → Drains into inferior vena cava.
- The left ovarian vein → Drains into the left renal vein.
Lymphatic drainage
It accompanies the ovarian vessels to reach the para-aortic LNs at the level of L2.
Nerve supply
- Sympathetic: from the lateral horn cells of spinal segmentT10.11.
- Parasympathetic: from the inferior hypogastric plexus (pelvic splanchnic nerve, S2,3,4).
Histological structure of the ovary
A section through the whole ovary shows that it is formed of a broad outer cortex, and a smaller inner medulla. The cortex and medulla grade into one another without a clear line of demarcation.
The ovarian medulla: is composed of loose connective tissue stroma rich in elastic fibers and contains numerous large blood vessels, lymphatics and nerves
The ovarian cortex: The cortex of the ovary is highly cellular. It contains large numbers of ovarian follicles embedded in the cellular stroma. The cortex is composed of the following:
I. The germinal epithelium: a continuous sheet of low cuboidal epithelium covering the surface of the ovary. It is named with respect to the earlier theory which considered this layer as the origin of the primordial germ cells. Update theories have proved that the primordial germ cells have an extra-gonadal origin The germinal epithelium is continuous with the mesothelium covering the mesovarium.
II. Tunica albuginea: it lies immediately underneath the germinal epithelium. It is formed of condensed collagen fibers oriented parallel to the surface of the ovary.
III. Stromal cells: they are long spindle-shaped cells, embedded in a network of delicate collagen fibers (ovarian stroma).
IV. Ovarian follicles: they are the microenvironment for the development of female germ cells, the oocytes. These are:
- Primordial follicles:
- Growing follicles include primary follicles (unilaminar and multilaminar primary follicles), and secondary follicles (antral follicles).
- Mature Graafian follicles.
- Atretic follicles.
A. Primordial follicles
In the early embryonic life, the oogonia, female germ cells migrate to the cortex of the developing ovary, proliferate by mitosis and differentiate into large primary oocytes. During the third month of intrauterine life, the primary oocytes enter the first meiotic division and become arrested at the prophase stage throughout childhood till puberty.
Primordial follicles are characterized by the following:
- They are the only kind of follicles present in the ovarian cortex before puberty.
- They are numerous, small follicles located in the superficial part of the ovarian cortex beneath the tunica albuginea.
- Each follicle is formed of the primary oocyte surrounded by a single layer of flattened follicular cells (derived from ovarian stroma) and separated from the surrounding ovarian stroma by a basal lamina.
B. The growing follicles
At the age of puberty and under the effect of FSH on the anterior pituitary, a group of the primordial follicles are stimulated to change into growing follicles and the ovarian cycle begins.
The growing follicles include:
1. Primary follicles:
They are characterized by the following:
They are found in the outer zone of the cortex. As the follicles grow they sink. progressively deeper in the ovarian cortex. The primary oocyte becomes larger and the follicular cells grow into a single layer of cuboidal cells forming the unilaminar primary follicle.
Later on, the follicular cells proliferate to form two or three layers of stratified granulosa cells forming the multilaminar primary follicle, The oocyte becomes separated from the surrounding granulosa cells by a layer of glycoprotein stained with PAS, called the zona pellucida, secreted mainly by the oocyte.
Zona pellucida is traversed by microvilli projecting from the oocyte and granulosa cells via which communicating gap junctions between them occur. The glycoproteins of zona pellucida carry receptors for the fertilizing sperms and can induce the acrosomal reaction, The surrounding stromal cells become densely-packed around the follicle forming a limiting layer called the theca folliculi.
2. Secondary (antral) follicles:
They are characterized by the following:
The follicles increase in size, till it reaches about 200 μm in diameter. The granulosa cells proliferate rapidly forming from 6-10 layers around the oocyte. Immediately surrounding the zona pellucida, there is a layer of closely adherent low columnar granulosa cells called the corona radiata.
A clear fluid, the liquor folliculi accumulates in multiple intercellular spaces between the granulosa cells. it contains hyaluronic acid and a high concentration of estrogen. The theca folliculi becomes differentiated into:
- Theca interna is formed of a large number of blood capillaries and steroid-secreting cells which produce a precursor steroid that is further converted by the granulosa cells to release estrogen hormone.
- Theca externa which is formed of collagen fibers and stromal cells e.g. fibroblasts.
C. The mature Graafian follicle (tertiary follicle)
It is characterized by the following:
This preovulatory follicle is about 1cm or more in diameter and extends through the full thickness of the ovarian cortex. It can be seen by the naked eye as a transparent vesicle that protrudes against the tunica albuginea of the ovary. As liquor folliculi increases in amount, the spaces unite with each other forming a single crescentic cavity, the follicular antrum.
Since the granulosa cells do not multiply in proportion to the accumulation of liquor, the antrum folliculi increases in size while the granulosa cells form a thin layer around the antrum. The oocyte with its corona radiata lies eccentrically in the follicle, surrounded by a thickening of granulosa cells: cumulus oophorus projecting into the antrum.
The oocyte grows and acquires more organelles, multiple Golgi apparatuses, extensive mitochondria rER, many mitochondria, and numerous small vesicles. The Graafian follicle is surrounded by well-developed theca interna and externa.
D. Atretic follicles
Atretic follicles occur at any stage of follicular development (pre-and postnatal, till a few years after menopause). During the reproductive life of the women (30-40 years), only one ovum is liberated by the ovaries in each menstrual cycle. So the total number of ova liberated is about 400-450 i.e. not all ovarian follicles will develop to mature Graafian follicles but most of them become atretic follicles.
Atresia is the name for the degenerative process by which oocytes die without having been expelled by ovulation. It involves apoptosis of follicular cells and resorption of oocytes, followed by fibrous tissue formation. After a period depending on the size of the atretic follicle, it dissolves and becomes replaced by the ordinary stromal tissue of the ovary.
Oogenesis and maturation of the primary oocyte:
Just before ovulation the primary oocyte. containing the diploid number of chromosomes (46 d-chromosomes), grows and completes the first meiotic division giving rise to two unequal daughter cells, each cell contains 23 d chromosomes, these are the first polar body and the secondary oocyte.
Immediately after ovulation, the secondary oocyte starts the second meiotic division which will be completed only when fertilization occurs resulting in a mature ovum and the second polar body, each contains haploid chromosomes (23 s-chromosomes).
You can download Science online application on google play from this link: Science online Apps on Google Play
Female reproductive system organs, functions, anatomy & Histological structure of the uterus
Fallopian tubes function, location, anatomy & Histological structure of vagina
Monthly ovarian cycle, Corpus luteum & menstrual cycle phases, function & hormones
Ovarian hormones, Menopause, Functions of estrogen & progesterone in pregnancy
Female mammary glands (breast), signs of breast cancer & Mammary gland abnormalities