Osmolality, Concentrating mechanism of the kidney, Urine concentration and dilution
For the cells of the body to function properly, they must be bathed in the extracellular fluid with a relatively constant concentration of electrolytes and other solutes, The total concentration of solutes in the extracellular fluid, and therefore the osmolality, is determined by the amount of solute divided by the volume of the extracellular fluid, Thus, to a large extent, extracellular fluid sodium concentration and osmolality are regulated by the amount of extracellular water.
Urine concentration and dilution
The total body water is controlled by:
- The fluid intake which is regulated by factors that determine thirst, and
- The renal excretion of water which is controlled by multiple factors that influence glomerular filtration and tubular reabsorption.
Osmolality
Osmolality is a measure of the total concentration of discrete solute particles in solution, Posm= Osmolality of electrolytes + osmolality of glucose + osmolality of urea, The normal osmolality of the extracellular & intracellular fluids is about 300 milliosmoles per kilogram of water.
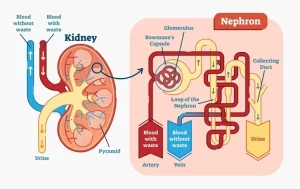
Concentrating mechanism of the kidney
In order to excrete the excess of ingested electrolytes, or in case of inadequate water supply, the kidney excretes concentrated urine, so that excess solutes are eliminated with a little loss of water from the body, The basic requirements for forming concentrated urine are:
- The level of ADH which increases the permeability of the distal tubules and collecting ducts to water, thereby allowing these tubular segments to eagerly reabsorb the water.
- A high osmolality of the renal medullary interstitial fluid which provides the osmotic gradient necessary for the water reabsorption to occur in the presence of high levels of ADH.
Renal medullary interstitium surrounding the collecting ducts is normally hyperosmotic; so, when ADH levels are high, water moves through the tubular membrane by the osmosis into the renal interstitium; and it is carried away by the vasa recta back into the blood, so, the urine concentrating ability is limited by the level of ADH and by the degree of the hyperosmolality of the renal medulla, The process by which the renal medullary interstitial fluid becomes hyperosmotic involves the operation of the countercurrent mechanism.
Countercurrent mechanism
The counter-current system is a system in which the inflow runs parallel, counter to, and adjacent to the outflow, The countercurrent mechanism depends on the special anatomical arrangement of the loops of Henle and the vasa recta, the specialized peritubular capillaries of the renal medulla, In human, about 25 percent of the nephrons are juxtamedullary nephrons with the loops of Henle and vasa recta that go deeply into the medulla before returning to the cortex.
Some of the Henle loops dip all the way to the tips of the renal papillae that project from the medulla into the renal pelvis, Paralleling the long Henle loops are the vasa recta, which also loop down into the medulla before returning to the renal cortex.
And finally, the collecting ducts, which carry the urine through the hyperosmotic renal medulla before it is excreted, also play a critical role in the countercurrent mechanism, The first step in the concentration of the urine is to create the hyperosmolality of the medullar interstitial fluid, Four different solute-concentrating mechanisms are responsible for this hyperosmolality.
- The principal cause is the active transport of sodium ions with the secondary active transport of chloride, and potassium ions out of the thick portion of the ascending limb of the loop of Henle into the outer medullary interstitial fluid, This increases the osmolality of the medullary interstitial fluid.
- Passive reabsorption of sodium and chloride ions from the thin ascending limb of the loop of Henle, This passive reabsorption process depends up on the prior existence of the medullary gradient to reabsorb water from the thin descending limb, thereby, increasing the concentration of sodium and chloride ions in the tubular fluid delivered to the thin ascending limb.
- ADH helps reabsorption of urea from the inner medullary part of the collecting ducts, This part becomes moderately permeable to urea and highly permeable to water, water is rapidly reabsorbed and this greatly increases urea concentration, Urea diffuses by concentration gradient through the collecting duct into the medullary interstitium; its concentration in the medullary interstitium is increased and increases the inner medullary fluid osmolality.
- Active reabsorption of sodium from the collecting ducts into the medullary interstitial fluid is associated with electrogenic passive absorption of chloride ions.
The net result of these four mechanisms is an increase in the osmolality of the medullary interstitial fluid to 1200-1300 mOsm/kg water in the pelvic tip of the medulla, The combination of these mechanisms is called the “counter-current multiplier mechanism” because it multiplies or increases the osmolality of the renal medullary interstitial fluid, When the concentration of ADH is high, the epithelium of the late part of the distal convoluted and the collecting duct becomes highly permeable to the water and the water is reabsorbed into the highly concentrated medullary interstitial fluid.
Counter-current exchange mechanism
The medullary blood flow has two characteristics for maintaining the high solute concentration in the medullary interstitial fluid constant.
- The medullary blood flow is very small in quantity, amounting to only 1-2 percent of the total blood flow of the kidney, Because of this very small and sluggish flow, the removal of solutes is minimized.
- The vasa recta functions as a counter-current exchanger that prevents the washout of solutes from the medulla.
Operation of vasa recta as counter-current exchangers in the kidney
As the blood flows down the descending limb in the vasa-recta, its osmolality is slightly lower than the osmolality of the medullary interstitial fluid, so, sodium chloride and urea diffuse from the interstitial fluid into the blood, while the water diffuses out into the interstitium, The osmolality of the blood in the vasa recta increases to 1200 mosm/kg water at its tip.
Then, as blood flows back up in ascending limb, the osmolality of the blood is slightly higher than the osmolality of the medullary interstitial fluid, so sodium chloride and urea diffuse, back out of the blood into the interstitium and water diffuses back into the blood, Thus, the blood of the vasa-recta removes a little amount of solutes from the interstitial fluid.
Diluting mechanism of the kidney
The late distal tubule and the collecting ducts are impermeable to the water when the antidiuretic hormone is not present in the circulating body fluids, In the case of hemodilution, absorption of solutes only takes place at these sites as the antidiuretic hormone is not secreted, and it is present in a low concentration.
At the thick portion of the loop of Henle, and the first segment of the distal tubule (diluting segment) there is active absorption of sodium ions and secondary active absorption of chloride and potassium ions, The osmolality of the fluid in the ascending limb of the Henle loop decreases progressively to about 100 milliosmoles per kg water by the time the fluid leaves this tubular segment.
In the late distal tubule and collecting ducts, there is an active absorption of sodium and passive absorption of anions e.g. chlorides, The osmolality of the tubular fluid decreases as little as 65-70 milliosmoles per Kg water by the time it leaves the collecting duct to enter the urine.
To summarize, the process for excreting dilute urine is one of absorbing solutes at the distal segments of the tubules, while water fails to be reabsorbed.
Functions of the loop of Henle, distal tubules, collecting ducts & Glucose tubular maximum
Transport through Renal tubules, Kidney Transport & function of proximal convoluted tubules
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
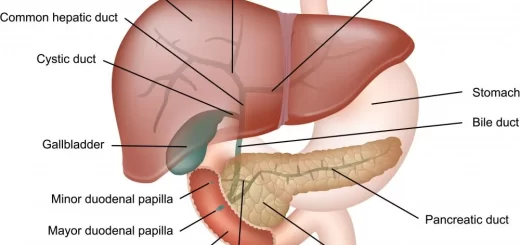
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
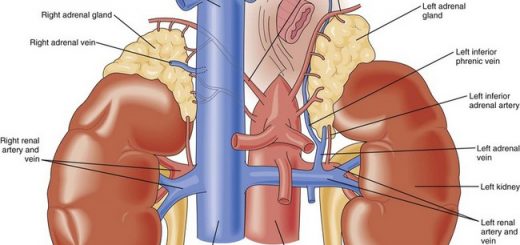
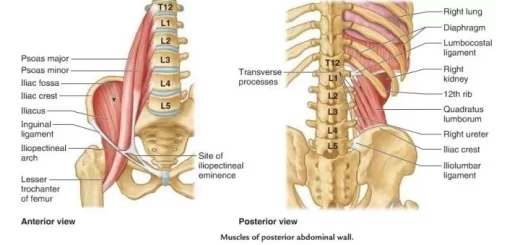
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play