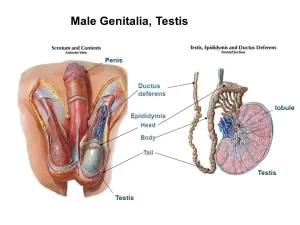
Organs of male genital system, Structure of the testis, Functions of Sertoli cells & Leydig cells
The male genital system consists of External genital organs ( Penis, and Scrotum), and Internal genital organs (Two testes, Two epididymides, Two vas deferens, Two seminal vesicles, Two ejaculatory ducts, and the Prostate), The male reproductive functions are spermatogenesis or the formation of sperms in the testis, the secretion of male sex hormones from the testis, and performance of the male sexual act.
Organs of Male genital system
Scrotum
- It is a dark skin fold situated at the lowermost part of the anterior abdominal wall.
- Its cavity is divided into 2 compartments by an incomplete fascial septum.
- Each half contains a testis.
- The scrotum is formed of skin and superficial fascia,
- The superficial fascia is differentiated into two layers.
- Superficial layer: It contains no fat, but contains Dartos muscle (an involuntary muscle that is supplied by sympathetic fibers which cause skin wrinkling in cold weather).
- Deep membranous layer (Colle’s fascia).
Penis
It is the external male genital organ for micturition and sexual intercourse.
Penis parts
- The root of penis: It is the attached part of the penis which is situated in the superficial. perineal pouch. It consists of: bulb and 2 crura. The bulb is the proximal expanded part of the corpus spongiosum, The crura are the proximal part of the corpus cavernosus They are firmly attached to the periosteum of the pubic arch.
- Body: It is the free part of the penis; its most anterior area is called the glans penis.
Arterial supply of the penis
The first three arteries arise from the internal pudendal. The last one arises from the femoral artery. All of them are paired:
- Dorsal artery of penis: for the glans penis and it lies on each side of the deep dorsal vein.
- Deep artery of penis: (cavernosal artery): for the corpus cavernosum and it lies in the corpus cavernosum.
- Artery of bulb: for the bulb and corpus spongiosum. It lies on each side of the urethra.
- Superficial external pudendal artery: for the skin and fascia.
Venous drainage
- Superficial dorsal vein of penis …. superficial to fascia penis.
- Deep dorsal vein of penis ……. deep to fascia penis.
Lymphatic drainage: to superficial inguinal lymph nodes.
Histological structure of penis
A)- The coverings: (mentioned from external to internal)
- Skin
- Superficial fascia: formed of a superficial layer of loose connective tissue, and a deep layer of dense fascia penis that envelops the erectile tissue.
B)- Erectile tissue: The erectile tissue consists of three elongated cylindrical masses; embedded in the fascia penis. The erectile tissue contains cavernous spaces which are formed of vascular channels, lined by continuous endothelium.
Corpora cavernosa
- Number& position: two dorsal lying side by side separated by an incomplete median septum and are surrounded by thick tunica albuginea.
- Distal expansion: not expanded.
- Traversing structure: helicine arteries (from the deep artery of the penis) are present in between the cavernous spaces.
- Cavernous spaces: irregular, larger at the center separated by dense fibro-elastic CT with many trabecular smooth muscle fibers.
- Rigidity during erection: they become very rigid due to the engorgement of the cavernous spaces with blood, helped by compression of the venous drainage against the tough tunica albuginea.
Corpus spongiosum
- Number& position: single, ventral and surrounded by thin tunica albuginea.
- Distal expansion: it forms the glans penis. In uncircumcised men, the glans is covered by a fold of thin skin, and the prepuce
- Traversing structure: penile urethra is present in the center, a common passage of urine and semen in male.
- Cavernous spaces: regular, equally-sized. Separated by more elastic CT trabeculae and less smooth muscle fibers.
- Rigidity during erection: less rigid, keeps the penile urethra patent during erection to allow semen ejaculation.
Testis
They are 2 flattened, oval glands 5 cm long, 3 cm wide and 2 cm thick in the adult male, suspended by the spermatic cords in the scrotum.
Testis presents 2 borders; anterior and posterior.
Posterior border: is related to:
- Epididymis, laterally
- Vas deferens, medially
Arterial supply of the testis: Testicular artery arises from the abdominal aorta opposite the 2nd lumbar vertebra.
Venous drainage by the testicular vein to:
- The left testis drains into the left renal vein.
- The right testis drains into the inferior vena cava
Lymphatic drainage: para-aortic lymph nodes at the level of the L2.
Anatomical and Histological structure of the testis
I)- Covering of the testis
Each testis is covered by many layers arranged from outside as follows
- Skin.
- Dartos muscle.
- Colle’s fascia (membranous layer of superficial fascia).
- External spermatic fascia, which is derived from the external oblique aponeurosis
- Cremasteric muscle and fascia, which are derived from the internal oblique muscle.
- Internal spermatic fascia, which is derived from fascia transversalis.
- Tunica vaginalis.
- Tunica albuginea.
- Tunica vasculosa.
Tunica vaginalis. a double-layered serous sac that encloses the testis that is picked up from the peritoneum during the descent of the testis into the scrotum leading to the formation of parietal and visceral layers.
Tunica albuginea: a thick fibrous connective tissue capsule under the tunica vaginalis. It is thickened at the back to form the mediastinum testis, through which the blood vessels enter and vasa efferentia leave the testis. Thin fibrous septa radiate from the mediastinum to divide the testis into incomplete testicular lobules.
Tunica vasculosa: a highly vascular loose connective tissue that lies beneath the tunica albuginea and extends into the testicular interstitium between the seminiferous tubules.
II) The seminiferous tubules
These are the structural and functional units of the testis, comprising its exocrine portion that produces spermatozoa. Each one is a coiled non-branching loop. terminating as the straight tubuli recti.
In the transverse section: They are roughly circular structures with a narrow lumen. Each tubule has a well-defined basal lamina and is surrounded by several layers of peritubular myoid cells (smooth muscle-like cells) and fibroblasts forming the tunicapropria. In between the tubules, the tunica vasculosa contains groups of eosinophilic interstitial cells (of Leydig), lymphatics, and nerves.
III) The seminiferous epithelium
The seminiferous tubules are lined by 2 types of cells, the spermatogenic cells, the main cell population, and Sertoli cells.
A. Spermatogenic cells
They are e male germ cells arranged in successive layers from the basal lamina to the lumen. They are seen in various stages of differentiation as the following:
1. Spermatogonia
Origin: they are the stem cells.
Appearance in histological sections: they are small, round cells containing the diploid number of chromosomes.
- In sexually-immature testis, they are the only type of spermatogenic cells present in the seminiferous tubules forming several rows.
- In sexually-mature testis, they form 1-2 layers, resting on the basal lamina of the seminiferous tubules.
Fate: spermatogonia undergo successive mitotic divisions to maintain their number and give rise to primary spermatocytes.
2. Primary spermatocytes
Origin: at puberty, they arise from the mitotic division of spermatogonia.
Fate: enter the first meiotic division to give rise to secondary spermatocytes.
Appearance in histological sections: the largest spermatogenic cells, found in 2-3 layers next to spermatogonia. They have a large euchromatic nucleus containing a diploid number of chromosomes (as 46 d-chromosomes). They are frequently seen in the histological sections as the prophase of the first meiotic division lasts for several days in human.
3. Secondary spermatocytes
Origin: from the first meiotic division of primary spermatocytes.
Fate: they are smaller than primary spermatocytes containing the haploid number of chromosomes (23 d-chromosomes). They are rarely seen in histological sections as they quickly enter the second meiotic division to give rise to spermatids.
4. Spermatids
Origin: from the second meiotic division of the secondary spermatocytes.
Fate: do not divide anymore; they enter the process of spermiogenesis to be transformed into spermatozoa.
Appearance in histological sections: seen in 2 successive stages of maturation;
- Early spermatids, they are small, round with a central round nucleus containing the haploid number of chromosomes (23 s-chromosomes).
- Late spermatids, they become elongated with a dark nucleus. They are attached to the apices of Sertoli cells.
5. Spermatozoa
Origin: differentiated from the late spermatids.
Appearance in histological sections: they fill the lumen of seminiferous tubules and attach themselves to the apices of Sertoli cells.
B. Sertoli cells
They are the non-proliferating, non-spermatogenic cells of the seminiferous epithelium.
Histological features:
- Site in between spermatogenic cells, extending from the basal lamina to the lumen of the seminiferous tubules.
- Shape: tall, irregular pyramidal cells resting by their broad base on the basement membrane of the seminiferous tubules. They reach the lumen by their thinner apex where spermatids and spermatozoa are attached.
- Nucleus: Sertoli cell has a large, infolded nucleus, with a tripartite nucleolar apparatus (nucleolus is flanked by 2 rounded masses of heterochromatin).
- Cytoplasm: pale due to the presence of numerous lipid droplets and abundant SER. The Sertoli cell has several Golgi complexes, numerous lysosomes, and a well-developed cytoskeleton (microfilaments and microtubules) which provides structural support and facilitates the release of maturing sperms by the process of spermiation.
- Lateral boundaries: show extensive cytoplasmic recesses to support the different spermatogenic cells. Occluding junctions between adjacent Sertoli cells forming the blood-testis barrier above the level of the spermatogonia thus dividing the seminiferous epithelium into two completely-separated compartments.
Basal compartment, containing:
- Tunica vasculosa.
- Tunica propria.
- Spermatogonia.
Adluminal compartment, containing:
- Spermatocytes (primary & secondary)
- Spermatids.
- Sperms.
Functions of Sertoli cell
1. Nutrition and supportive functions: of the spermatogenic cells to help their transformation into spermatozoa.
2. Phagocytic function: phagocytosis of dead sperms and cytoplasmic residual bodies of the maturing spermatocytes.
3. Secretory function:
- Androgen-binding protein (ABP): this accumulates testosterone and maintains its high concentration in the seminiferous tubular fluid which is essential for the completion of the process of spermiogenesis.
- Inhibin: a hormone that inhibits the over-secretion of FSH.
- A small amount of estrogens: is required as one of the stimulatory factors in spermatogenesis
- A large amount of luminal fluid of seminiferous tubules which serves as a medium for sperm transport.
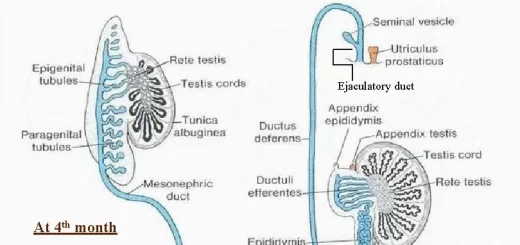
- Mullerian-inhibiting substance secreted during fetal development which causes regression of the Mullerian” ducts in males and induces descent of the testes to the inguinal region
4. Formation of blood-testis barrier:
- It isolates the antigenic-different germ cells from their own immune system of the adult male, thus prevents the autoimmune reaction against the developing spermatogenic cells.
- It protects the microenvironment of seminiferous epithelium from blood-borne harmful proteins and other macromolecules.
IV. Interstitial cells of Leydig
Histological features:
- Present in tunica vasculosa, either singly or in clusters, surrounded by fenestrated capillaries.
- They are large, polyhedral cells showing the LM & EM features of steroid-secreting cells with no secretory granules.
Function: Leydig cells secrete the steroid hormone, testosterone.
You can download Science online application on google play from this link: Science online Apps on Google Play
Testis functions, sperms production, Factors affecting spermatogenesis, Structure of Epididymis
Vas deferens function, histology, anatomy, Varicocele & Functions of Seminal vesicle
Prostate function, structure, lobes, Benign enlargement of prostate & malignant prostatic tumor
Divisions of Perineum, Fascia of Urogenital triangle & Contents of Ischiorectal fossa
Testosterone effects, low testosterone symptoms, Hypogonadism & Hypergonadism in male