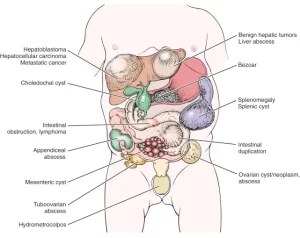
Masses in left hypochondrium and the epigastrium, Is an abdominal mass always cancer?
Masses in the left hypochondrium (the upper left region of the abdomen) can arise from various organs, including the spleen, stomach, kidney, pancreas, and colon.
Masses in left hypochondrium
Masses in the left hypochondrium (upper left abdominal region) can arise from various organs, including the spleen, stomach, colon, pancreas, kidney, and surrounding structures.
1. Splenic Causes
- Splenomegaly (enlarged spleen) – due to infections (e.g., malaria, mononucleosis), hematologic disorders (e.g., leukemia, lymphoma), or portal hypertension.
- Splenic cysts – congenital or secondary to trauma or infection.
- Splenic abscess – rare but can occur due to infections.
- Splenic tumors – benign (hemangioma, lymphangioma) or malignant (lymphoma, metastasis).
2. Gastrointestinal Causes
- Gastric tumors – including gastric carcinoma or gastrointestinal stromal tumors (GISTs).
- Colonic masses – such as left-sided colon cancer or diverticular abscess.
- Pancreatic tumors – tumors in the tail of the pancreas (e.g., adenocarcinoma, cystic neoplasms).
3. Renal Causes
- Left renal masses – such as renal cysts, renal cell carcinoma, or polycystic kidney disease.
- Perinephric abscess – infection around the kidney.
4. Other Causes
- Retroperitoneal tumors – liposarcoma, lymphoma, or other soft tissue tumors.
- Diaphragmatic hernia – protrusion of abdominal contents into the chest cavity.
- Lymphadenopathy – enlarged lymph nodes due to infections or malignancies.
Evaluation & Diagnosis
To determine the cause of a left hypochondrial mass, investigations may include:
- Ultrasound (USG).
- CT scan or MRI.
- Blood tests (CBC, tumor markers, infection markers).
- Endoscopy (if a gastric cause is suspected).
- Biopsy (if malignancy is suspected).
1. Spleen
Criteria of splenomegaly:
- intra-abdominal.
- mobile with respiration.
- can’t insinuate the hand between it and left costal margin “Hook sing”.
- direction of growth: towards right iliac fossa from LT costal margin” because of phrenicocolic ligament.
- firm with smooth surface 6-renal angle empty.
- anterior border with a characteristic notch.
- Dull and its dullness is continuous with normal spleen dullness 9- spleen has to enlarge three times to be palpable clinically.
Causes of Splenomegaly
- Infectious: Protozoa: (Bilhariziasis, Malaria). Viral (CMV, EBV). Bacterial :(Septicemia, TB, Typhoid).
- Cellular infiltration: (Amyloidosis, sarcoidosis).
- Collagen disease: Felty’s.
- Space occupying lesions: Hydatid cyst.
- Cellular proliferative: (Leukemia, Lymphoma, Spherocytosis, hemolytic anemia, Myelofibrosis, sarcoidosis)
- Infarction, trauma: (Splenic hematoma).
2. Left-Sided Colonic Mass:
- It is mobile, nodular, and resonant.
- It does not move with respiration.
- It is commonly due to carcinoma colon.
3. Left Renal Mass from Upper Pole of any Cause.
4. Left-Sided Adrenal Mass
- It does not move with respiration. It is not mobile.
- It is a deeply placed mass. Often, it crosses the midline.
- It is resonant on percussion. It mimics kidney mass.
5. Mass arising from the Tail of the pancreas
- Clinical features are the same as other pancreatic masses.
- The causes are pseudocyst in the tail of the pancreas and cystadenomas.
Masses in the epigastrium
1. Palpable Left Lobe of the Liver
- It is in the epigastric region.
- Its upper border cannot be felt.
- It moves with respiration.
- It extends towards the left hypochondrium.
- It is dull on percussion.
2. Stomach mass
Features of Stomach Mass
- It is located in the epigastric region.
- It moves with respiration. It is intra-abdominal
- It is resonant or impaired resonant on percussion.
- Mass may be better felt on standing or on walking.
- Mass is often mobile, unless it gets adherent posteriorly.
- In pylorus mass, all margins are well felt which is mobile with features of gastric outlet obstruction.
- Mass from the body of the stomach is horizontally placed without any features of obstruction.
- Mass from the upper part of the stomach near the OG junction causes dysphagia.
- Mass from the fundus of the stomach is in the upper part of the epigastric region towards the left side.
- Carcinoma stomach is nodular and hard. It is the most common cause for stomach mass.
- Leiomyoma of the stomach is smooth and firm.
Management of gastric carcinoma
- Early growth or pylorus→ lower radical gastrectomy with removal of tumor, proximal 5cm clearance, nodal clearance, greater and lesser omentum, distal pancreas and spleen (now not regularly removed; it is removed to clear splenic nodes – one of the node stations) and Billroth II anastomosis or Roux-en-Y anastomosis is done.
- Postoperatively, adjuvant chemotherapy should be given → 5 fluorouracil, mitomycin, epirubicin, cisplatin.
- Growth in body, proximal growth, diffuse carcinoma and generalized linitis plastica→total radical gastrectomy with oesophagojejunal anastomosis.
- Neoadjuvant chemotherapy in advanced gastric cancer prior to surgery and later gastrectomy
- Instillation of mitomycin C impregnated charcoal intraperitoneally to control lymphatic disease (Japan).
- Palliative procedures like palliative partial gastrectomy, anterior gastrojejunostomy, Devine’s exclusion procedure, luminal stenting in proximal inoperable growths, and chemotherapy are used in inoperable cases.
- In early carcinoma, proper lymph nodal clearance is important.
- Rare cause of epigastric mass “not cancer” this case occur in patient with psychological trouble patients and stomach become full of hair.
3. Abdominal masses of pancreatic origin:
1- solid mass
- endocrine tumor.
- cancer head or body of pancreas either metastatic or local advanced.
2 – cystic
- neoplastic: neoplasm WOPN (walled-off pancreatic necrosis).
- Inflammatory: acute fluid collection and after maturation became pseudocyct. acute necrotic collection and after maturation become walled of necrosis.
3. WOPN (walled-off pancreatic necrosis)
Pseudocyst of the Pancreas
- Mass in the epigastric region. It is smooth and soft. It can be tender if it is infected.
- It does not move with respiration.
- It is not mobile.
- It has transmitted pulsation. It is confirmed by placing the patient in a knee-elbow position.
- The lower border is well felt. The upper border is not clear.
- It is resonant on percussion.
- Baid test: As the stomach is pushed in front, Ryle’s tube, when passed, can be felt per abdomen on palpation.
- appear several weeks after the onset of pancreatitis.
- They are to be distinguished from acute fluid collections, walled of necrosis, and abscesses.
Classification:
Non-necrotizing → 80%, Ntibiotics not required.
Necrotizing →20%.
- 70%….infected necrosis.
- Start antibiotics.
- 80%…. deaths.
- Absolute indication for surgery.
Pseudocycts distinguation from other cystic:
- lack of epithelial lining.
- high concentration of enzymes.
- formation after 4 weeks from the episode of acute pancreatitis.
Investigations for pseudocyst of pancreas
- Ultrasound is a commonly done procedure.
- CT scan ideal and choice.
- LFT, serum amylase, prothrombin time.
- ERCP to find out communications.
- Barium meal-not done now-shows widened vertebrogastric angle.
Complications
- Rupture-3%.
- Infection-20%.
- Bleeding-torrential 7%.
- Cholangitis.
Management:
- In the absence of symptoms, It is safe to manage acute or chronic pseudocysts without intervention.
- In the presence of symptoms: Wait for 6-12 weeks for Cyst maturation before endoscopic or surgical drainage.
Indications of intervention:
- Cyst size bigger than 6 cm.
- Mature thick wall cyst. Infected cyst.
Interventions
- Roux en Y cystojejunostomy is ideal.
- Cystogastrostomy-Jurasz procedure- commonly done cystoduodenostomy.
- Cystogastrostomy with external drainage if infected Smith operation.
- Endoscopic stenting.
- Laparoscopic cystogastrostomy− popular− safer.
- Guided aspiration helps but has a high recurrence rate of 70%.
Pancreatic cyst adenocarcinoma
- Mass is smooth, firm, does not move with respiration, nonmobile, resonant on percussion.
- The patient complains of back pain.
Serous cystadenomas (SCAs)→
- Have thick, fibrous walls and contain clear fluid.
- Almost all SCAs are benign.
Intraductal Papillary Mucinous Neoplasms (IPMNs)→
- Start in the ducts that connect the pancreas to the intestine.
- They’re the most common type of precancerous cyst.
- They produce large amounts of proteins that form mucus (mucin) in the cyst lining and fluid.
- It’s difficult to predict if and when an IPMN will become cancerous, although research indicates that those that involve the main pancreatic duct are at higher risk for this.
Murmous Cystic Neoplasms (MCNs)→
- These cysts are precancerous growths that can start in the body and tail of the pancreas.
- They almost always develop in women rather than men.
- Large ones that contain tiny walls that divide the cyst into compartments, called septations, may be more likely to become cancerous.
Pancreatic Cancer (Advanced cancer head pancreas, cancer body pancreas)
- It is the fourth leading cause of cancer deaths, being responsible for 8% of all cancer–related deaths.
- Approximately 75% of all pancreatic carcinomas occur within the head or neck of the pancreas, 15-20% occur in the body of the pancreas, and 5-10% occur in the tail.
- Advanced intra-abdominal disease: Presence of ascites, a palpable abdominal mass, hepatomegaly from liver metastases, or splenomegaly from portal vein obstruction.
- Advanced disease: Para-umbilical subcutaneous metastases (or Sister Mary Joseph nodule).
- Possible presence of palpable metastatic mass in the rectal pouch (Blumer shelf).
- Possible presence of palpable metastatic cervical nodes: Nodes may be palpable behind the medial end of the left clavicle (Virchow node) and other areas in the cervical region.
4. Colonic Mass
- It is due to carcinoma of the transverse colon.
- It is a mobile, horizontally placed, nodular, hard mass which does not move with respiration. Caecum will be dilated and palpable.
- It is resonant or impaired resonant on percussion.
- The patient will be having bowel symptoms, loss of appetite and decreased weight.
5. Para-aortic Lymph Node Mass
- Mass in the epigastric region, which is deeply placed, nonmobile, not moving with respiration.
- It is vertically placed above the level of the umbilicus and resonant on percussion.
- Causes for enlargement are: Secondaries, lymphomas, or tuberculosis.
6. Aortic Aneurysm
It is smooth, soft, and pulsatile (expansile pulsation, which is confirmed by placing the patient in a knee-elbow position). It is vertically placed above the level of the umbilicus, nonmobile, not moving with respiration, and resonant on percussion.
You can subscribe to Science Online on YouTube from this link: Science Online
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion