Malabsorption syndrome causes, Symptoms, Treatment and How do you fix malabsorption syndrome?
Malabsorption syndrome is a digestive disorder that prevents your body from effectively absorbing nutrients from the food you eat. This occurs primarily due to damage to the small intestine, where most nutrient absorption takes place.
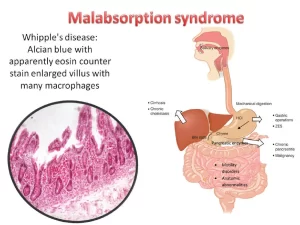
Malabsorption syndrome
It is a clinical syndrome in which there is malfunction, digestion, and absorption of the food intake by the oral route.
Types
- Pan-malabsorption: Here malabsorption to all nutrient intake (GLOBAL).
- Specific Malabsorption: Either malabsorption to an individual nutrient or class of nutrients. (PARTIAL).
In general, the digestion and absorption of food materials can be divided into three major phases: luminal, mucosal, and postabsorptive.
Physiology of absorption and digestion
- Intraluminal Phases.
- Mucosal Phase.
- Absorptive phase.
Intraluminal phases
Fats
- Pancreatic enzymes (lipase and colipase) split long-chain triglycerides into fatty acids and monoglycerides, which combine with bile acids and phospholipids to form micelles that pass through jejunal enterocytes.
- Absorbed fatty acids are resynthesized and combined with protein, cholesterol, and phospholipids to form chylomicrons, which are transported by the lymphatic system.
- Medium-chain triglycerides are absorbed directly.
- Unabsorbed fats trap fat-soluble vitamins (A, D, E, K) and possibly some minerals, causing deficiency. Medium chain triglycerides MCT are absorbed directly into portal blood without the need for micellar formation.
- The pancreatic lipase requires PH 8 to be active. Hyperacidity inactivates the pancreatic lipase. Although pancreatic function is required for fat digestion, a person may lose nearly 90 of lipase output from the pancreas before the efficiency of fat digestion and absorption is affected.
- Decreased bile salt concentration may be due to biliary obstruction or liver disease lead to mild steatorrhea.
- Other causes of impaired micelle formation as bile salts deconjugation, Impaired enterohepatic bile circulation, as seen in small bowel resection or regional enteritis.
- Bacterial overgrowth results in deconjugation and dihydroxylation of bile salts, limiting the absorption of fats.
- Unabsorbed bile salts stimulate water secretion in the colon, causing diarrhea.
Protein
- Initial breakdown started by gastric pepsins activated by PH 1-3 and inactivated at PH>5. Gastric pepsin also stimulates the release of cholecystokinin which is critical to the secretion of pancreatic enzymes.
- Enterokinase: a brush border enzyme, activates trypsinogen into trypsin, which converts many pancreatic proteases into their active forms.
- Active pancreatic enzymes hydrolyze proteins into oligopeptides, which are absorbed directly or hydrolyzed into amino acids.
- Additional mucosal brush border oligopeptides further cleave small peptides, with free amino acids and oligopeptides.
CHO
- Salivary and pancreatic amylases hydrolyze starch into mono and disaccharides.
- The brush border enzymes hydrolyze the disaccharides into monosaccharides (glucose, galactose, and fructose).
- Fructose is transported by facilitated diffusion, but glucose and galactose are transported by a sodium-dependent active transporter (SGL-1).
- Colonic bacteria ferment unabsorbed carbohydrates into carbon dioxide, methane, hydrogen, and short-chain fatty acids (butyrate, propionate, acetate, and lactate). These fatty acids cause diarthea. The gases cause abdominal distention and bloating.
Mucosal phase
- This phase needs sufficient intact area, also, intact brush border enzymes They are important in the hydrolysis of disaccharides. (Lactase deficiency of the brush border leads to lactose intolerance).
- Lactase deficiency, either primary or secondary, is the most common form of disaccharidase deficiency, Secondary lactase deficiency can result from acute gastroenteritis (rotavirus and giardia infection), chronic alcoholism, celiac sprue, radiation enteritis, regional enteritis, or acquired immunodeficiency syndrome (AIDS) enteropathy.
- This phase lesion is either due to: Primarily mucosal disease or resection of part of the intestine.
Absorptive phase
In the postabsorptive phase, reassembled lipids and other key nutrients are transported via the lymphatics and portal circulation from epithelial cells to other body parts. Lymphatic obstruction leads to impaired chylomicrons and lipoproteins.
Clinical picture
Fats
- Steatorrhea
- Watery diarrhea due to the osmotic effect of non-absorbed short-chain fatty acids.
- Weight loss.
- Vitamin A, E, D, K deficiency manifestations.
- The stool is bulky, greasy, and malodorous and floats.
CHO
- Diarrhea (watery stool due to the osmotic effect of non-absorbed CHO).
- Weakness.
- Loss of weight.
- Distention due to fermentation of non-absorbed CHO in the colon by bacteria (gases, bloating).
- Milk intolerance.
- Stool PH is acidic <6 and increased stool osmotic gap.
- OGTT, after a standard dose of oral glucose low rise, is an indication of malabsorption.
- Breath hydrogen test: If CHO is not absorbed, fermentation by Colonic
- bacteria into hydrogen as a byproduct, exhaled by the lung. So increased hydrogen in the breath means malabsorption).
Protein
- Edema.
- Weight loss.
- Weakness and fatigue.
- Amenorrhea.
- Alpha 1 Antitrypsin clearance test (In protein-losing enteropathy).
Water
- Dehydration.
- Nocturnal urination due to delayed water absorption.
Diagnosis
Fecal fat estimation in 72-hour stool collection: Fecal fat estimation in 72-hour stool collection (Diet has 100 g of fat per day several days before stool collection) is diagnostic of fat malabsorption. Fecal fat excretion in healthy individuals should be less than 7 g/d). Severe fat malabsorption (fecal fat ≥ 40 g/day) suggests pancreatic insufficiency or small bowel mucosal disease. It is unacceptable to most patients and difficult to do.
- D-xylose test: D-xylose test can be useful to differentiate SB cause from pancreatic insufficiency.
- D-Xylose is absorbed by SB by passive diffusion and does not require pancreatic enzymes for digestion and is excreted in urine.
SB cause can be investigated by biopsy, aspiration, and radiological images.
Pancreatic etiology by: CT, MRCP, H ERCP, and EUS to evaluate chronic pancreatitis changes.
A pancreatic enzyme supplements trial might be diagnostic.
The Schilling test
Assesses malabsorption of vitamin B12. Its 4 stages determine whether the deficiency results from pernicious anemia, pancreatic exocrine insufficiency, bacterial overgrowth, or ileal disease.
- Stage 1: The patient is given 1 mcg of radiolabeled Cyanocobalamin PO concurrent with 1000 mcg of Non-labelled Cobalamin IM to saturate hepatic binding sites. A 24-hour urine collection is analyzed for radioactivity; urinary excretion of < 8% of the oral dose indicates malabsorption of cobalamin.
- Stage 2: If stage 1 is abnormal, the test is repeated with the addition of an intrinsic factor. Pernicious anemia is present if the intrinsic factor normalizes.
- Stage 3: It is done after adding pancreatic enzymes; normalization in this stage indicates Cobalamin malabsorption secondary to pancreatic insufficiency.
- Stage 4: It is done after antimicrobial therapy with anaerobic coverage normalization after antibiotics suggest bacterial overgrowth.
Cobalamin deficiency Secondary to ileal discase or ileal resection results in abnormalities in all stages.
Symptoms of Malabsorption
Symptoms can vary depending on which nutrients aren’t being absorbed, but common signs include:
- Digestive issues: Diarrhea, bloating, gas, abdominal pain, greasy or foul-smelling stools.
- Weight loss: Despite eating enough.
- Nutritional deficiencies: This leads to symptoms like fatigue, weakness, skin problems, hair loss, and bone pain.
- Anemia (hypochromic, microcytic).
- Anemia (macrocytic).
- Bleeding, bruising, petechiae.
- Carpopedal spasm.
- Edema.
- Glossitis.
Other symptoms
- Sometimes abdominal pain with the diarrhea.
- Aphthous ulcer (in Celiac disease).
- Raynaud’s phenomena.
Causes of malabsorption
1- Impaired digestion
- Primary pancreatic exocrine insufficiency: Removal, Chronic pancreatitis, Hemochromatosis, Cystic fibrosis, Tumor of the pancreas.
- Gastric surgery (Bliroth, pyloroplasty, gastroenterostomy, Vagotomy), gastrocolic fistula, Inadequate gastric mixing, rapid emptying, or both.
- Gastrinoma: due to the inactivation of the pancreatic enzymes by the hyperacidity.
2. Reduced bile salt
- Bacterial overgrowth.
- Liver disease.
- Ileal disease and resection.
3- Impaired absorption
Nutrient malabsorption is due to inherited or acquired defects:
- Inherited defects include glucose-galactose malabsorption, abetalipoproteinemia, cystinuria, and Hartnup disease or Sucrose-isomaltose deficiency.
- Acquired disorders are far more common and are caused by the following:
- Decreased absorptive surface area, as seen in intestinal resection of intestinal bypass.
- Damaged absorbing surface, as seen in celiac sprue, tropical sprue, Crohn’s disease, AIDS enteropathy, chemotherapy, or radiation therapy.
- Infiltrating diseases of the intestinal wall, such as lymphoma and amyloidosis.
- Infections, include bacterial overgrowth, giardiasis, Whipple disease, cryptosporidiosis, and microsporidiosis.
Immunoglobulin A (IgA) deficiency (the most common immunodeficiency) is due to decreased or absent serum and intestinal IgA, which clinically appears similar to celiac disease and is unresponsive to a gluten-free diet.
Acrodermatitis enteropathy is an autosomal recessive disease with a selective inability to absorb zinc, leading to villous atrophy and acral dermatitis.
Autoimmune enteropathy is primarily diagnosed in children presenting with intractable secretory diarrhea and villous atrophy. Autoimmune enteropathy occurs as a result of antibodies directed against intestinal epithelial and goblet cells. Additional cell types affected by autoantibodies include islet and parietal cells.
4- Lymphatic obstruction
e.g. lymphangiectasia and lymphoma.
5- Drugs
cholestyramine, neomycin, colchicine, irritant laxative.
6- Others
C.H.F, (congestion of the small intestine), carcinoid tumor, diabetes mellitus, adrenal insufficiency, thyroid disorders.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach