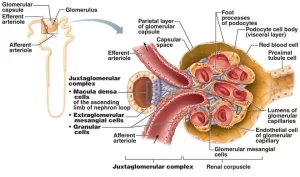
Juxtaglomerular apparatus structure, function and Autoregulation of glomerular filtration rate
The juxtaglomerular apparatus is located at the vascular pole of each glomerulus where the afferent and efferent arterioles come in close contact with the initial part of the distal convoluted tubule. It is made up of tubular and vascular elements of the nephron which interact to control the systemic blood pressure and the rate of glomerular filtration (and hence the rate of urine formation).
Histological components of juxtaglomerular apparatus
A. Juxtaglomerular (JG) cells
They are modified smooth muscle fibers in the tunica media of the afferent arteriole (occasionally in the efferent arteriole) as it enters the vascular pole of the glomerulus. Here, the internal elastic lamina of the afferent arteriole is lacking. They have the histological features of protein-secreting cells with prominent secretory granules.
Function:
- Synthesis and release of protein hormone, renin.
- Secretion of erythropoietin.
B. Macula densa cells
They are modified cells of the distal tubule that come in close contact with the afferent arteriole at the vascular pole of the glomerulus of its nephron.
Histological features: They differ from the ordinary cells of the distal tubule in the following:
- They are closely-packed columnar cells with crowded and superimposed nuclei.
- Thus, the cells appear as a dense spot (hence the name “macula densa”).
- The cytoplasm shows few mitochondria with no basal membrane infoldings.
- The apical cell membrane has numerous microvilli and a central cilium that acts as a sensor for sodium ion concentration in tubular fluid and for blood pressure changes.
- They extend a basal process to contact the juxtaglomerular cells by gap junctions to signal their release of the renin hormone.
Function: osmoreceptors.
C. Extra-glomerular mesangial cells (polar cushion cells or lacis cells)
These are groups of cells occupying the angle between the afferent and efferent arterioles.
Histological features: They are small cells with a lace-like network of cytoplasmic processes that contact the macula densa, the juxtaglomerular, and the intraglomerular mesangial cells by gap junctions for intercellular signaling.
Function: support and coordination function.
Functions of Juxtaglomerular Apparatus
- Endocrine function: (JG) cells secrete renin which leads to the formation of angiotensin Il that regulates the ABP. Moreover, the JG cells secrete erythropoietin hormone that stimulates erythropoiesis.
- Autoregulation of GFR and RBF.
Histological structure of the collecting ducts
The last part of each nephron is the short connecting tubule which carries the filtrate from the distal convoluted tubules into the cortical collecting ducts. These are located in the medullary rays and continue down through the medullary pyramid as medullary collecting ducts.
Many medullary collecting ducts join to form larger straight papillary ducts of Bellini, which open in the area cribrosa at the apex of the renal papilla. The lining cells are less eosinophilic with distinct intercellular boundaries. Two types of lining cells can be distinguished:
- Principal cells (light cells); they are the majority, present in all parts of collecting ducts. They are pale with few mitochondria and their function is ADH-regulated water facultative reabsorption.
- Intercalated cells (dark cells): they are few, found mainly in the smaller collecting ducts. They have dark cytoplasm with numerous mitochondria and their function is regulation of acid-base balance in the tubular fluid.
Autoregulation of glomerular filtration rate (Tubulo-glomerular Feedback)
Although a change in the mean arterial pressure causes a marked change in urinary output, this pressure can decrease to 75 mmHg or increase to 160 mmHg and cause very little change in glomerular filtration rate; this is called autoregulation of glomerular filtration rate.
It is important because the nephron requires an optimal rate of glomerular filtration to perform its function. As little as a 5 percent increase or decrease in glomerular filtration can have serious effects in causing either excess fluid loss in urine or too little excretion of the necessary waste products.
Mechanism of autoregulation of glomerular filtration rate
The mechanism of autoregulation is uncertain. It is intrinsic to the kidneys since autoregulation can be demonstrated in transplanted, denervated kidneys, There are two hypotheses (theories) trying to explain autoregulation of the glomerular filtration rate and renal blood flow.
One mechanism responds to changes in arterial pressure (Myogenic mechanism) and another that responds to changes in [NaCI] tubular fluid (Tubuloglomerular feedback mechanism), Both regulate the tone of the afferent arteriole.
Myogenic hypothesis
The afferent arterioles have the inherent ability to respond to changes in vessel circumference by contracting or relaxing – (a myogenic response), The myogenic hypothesis attributes the increase in renal vascular resistance that accompanies an increase in systemic arterial pressure to contraction of the afferent arteriolar smooth muscle in response to stretch.
On the other hand, a decrease in systemic arterial pressure decreases the stretch on the afferent arteriolar smooth muscle and leads to afferent arteriolar dilatation.
Juxtaglomerular hypothesis (Tubuloglomerular feedback (TGF) mechanism)
The juxtaglomerular hypothesis mechanism involves a feedback loop in which a change in GFR leads to alteration in the concentration of NaCl in tubular fluid, which is sensed by the macula densa of the juxtaglomerular apparatus and converted into signals that affect the afferent arteriolar resistance and thus the GFR.
A) In case of hypertension
- An increase in arterial pressure leads to an increase in glomerular capillary pressure, RPF, and GFR.
- The increase in GFR leads to increased delivery of Na+ Cl− to the macula densa cells of the juxtaglomerular apparatus.
- Macula densa cells will release a vasoconstrictor substance (e.g., ATP, adenosine & thromboxane), which causes vasoconstriction of the afferent arteriole and normalization of GFR.
The net effect is an increase in the afferent arteriolar resistance and a decrease in GFR, thereby counteracting the initial increase in GFR.
B) In case of hypotension
The Juxtaglomerular hypothesis attributes autoregulation of the glomerular filtration rate to two special feedback mechanisms:
- An afferent arteriolar vasodilator feedback mechanism.
- An efferent arteriolar vasoconstrictor feedback mechanism.
1. The afferent arteriolar vasodilator feedback mechanism
- A decrease in arterial pressure leads to a decrease in glomerular capillary pressure, RPF, and GFR
- The decrease in GTR leads to decreased delivery of Na+ Cl− to the macula densa cells of the juxtaglomerular apparatus.
- Macula densa cells will decrease the release of vasoconstrictor substances. The fall in ATP and adenosine, with the release of vasodilator substances like (NO) results in afferent arteriolar vasodilatation.
This increases the rate of blood flow into the glomerulus and increases the glomerular pressure, with a subsequent increase of GFR back to normal.
2. The efferent arteriolar vasoconstrictor feedback mechanism
- The low concentration of Na+ and Cl− ions causes the JG cells to secrete renin from their granules.
- The renin causes the formation of angiotensin II.
- Angiotensin Il constricts the efferent arterioles, which causes the pressure in the glomerulus to rise.
- The increased pressure then causes the glomerular filtration rate to return back to normal.
Autoregulation of renal blood flow
The renal blood flow is relatively constant between the limits of 70 and 160 mmHg mean arterial pressure. It is mainly the afferent arteriolar feedback mechanism that causes this renal blood flow autoregulation.
If the mean arterial pressure is increased:
- RBF and GFR are increased.
- The concentration of sodium and chloride ions at macula densa increases which causes afferent arteriolar constriction that decreases the GFR and RBF back to normal.
If the mean arterial pressure is decreased:
- The renal blood flow becomes too little, the glomerular pressure falls, and the GFR also decreases.
- The concentration of sodium and chloride ions decreases at the maculadensa which causes afferent arteriolar dilatation that increases the renal blood flow and GFR back toward normal despite the low arterial pressure.
When the arterial pressure remains low for more than 10 to 20 minutes: Blood flow autoregulation disappears. Instead, the efferent arteriolar vasoconstrictor mechanism becomes more potent which decreases the renal blood flow. This allows the glomerular filtration rate to remain almost constant, but the marked decrease in blood flow through the kidney helps to return the arterial pressure back to normal.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Suprarenal glands (adrenal glands) anatomy, structure & Effect of Deficiency of Catecholamines
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia