Incontinence of urine causes, types, treatment, and How to solve urine leakage problems?
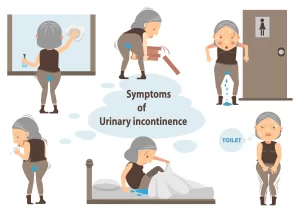
Urinary tract infections (UTIs) can cause an increased urge to urinate. Some medications may contribute to incontinence. Symptoms of Urinary Incontinence can vary depending on the type of incontinence but may include leaking urine, frequent urination, difficulty holding urine, and feeling a strong urge to urinate.
Incontinence of urine
Urinary incontinence is a common problem affecting millions of people, but it’s often a source of embarrassment and discomfort. It is the unintentional loss of bladder control, Urine leaks when pressure is put on the bladder, such as when coughing, sneezing, or exercising. A sudden, strong urge to urinate is followed by an involuntary loss of urine. The bladder becomes overly full and leaks. there is a combination of stress and urge incontinence.
Micturition centers
- The sacral micturition center at S2.3.4 and it is responsible for reflex micturition in neonates as the bladder fills with urine—-Sacral center —-efferent positive reflex to bladder—voiding.
- The pontine micturition center usually activates at the age of 2 y and it is responsible for holding of urinary external sphincter.
- The cerebral or limbic micturition center usually matures at 4-6 y of age and it controls the whole act of micturition and usually, it inhibits the act of micturition by negative impulse.
Micturition phases
- Filling phase: during this phase, there is no detrusor muscle contraction. if it happens, it is called involuntary or over-activity of the detrusor muscle.
- During the bladder filling or storage phase, the intravesical pressure gradually increases till 15 mmgh then with more increase in the volume of the urine the detrusor muscle also is more relaxed to accommodate more urine so there is no increase in intravesical pressure with an increase in the volume of urine, this is called urine compliance or viscoelasticity of bladder.
- As the bladder reaches the maximum capacity, there is no further elasticity and the pressure starts to increase till 40 mmgh where the limbic MC will facilitate the act of micturition and the sympathetic innervation will be blocked with relaxation of the bladder neck and external sphincter with over-stimulation of parasympathetic nerve causing voiding.
- At the end of micturition, the reverse will happen where the bladder neck will contract firstly then the inner portion of the external sphincter and another cycle of filling or storage will starts.
Definition: Involuntary escape of urine from the urethra.
1. Stress Incontinence
Incidence: In women after middle age with a history of repeated vaginal deliveries that result in a weak pelvic floor.
Cause: loss of the anatomic support of the urinary sphincters (from the weakened pelvic floor) with funneling of the bladder base.
Urodynamics: Reduced maximum urethral pressure with normal intravesical pressure.
Pathogenesis: a Sudden increase in abdominal pressure (during coughing, laughing or straining) causes the intravesical pressure to exceed the low maximum urethral pressure. This is accompanied by a bout of urine leak.
Treatment: By suspension of the bladder base to restore the anatomical support of the urinary sphincter. Once the position is restored, the sphincter mechanism usually regains its function. This is achieved by trans-vaginal application of a tension-free vaginal tape (TVT)) The tape passes from the anterior abdominal wall just above the symphysis pubis on one side, then behind the vesico-urethral junction and up to the anterior abdominal wall on the other side. This allows regained suspension of the vesico-urethral junction area, and restoration of the anatomical support of the urinary sphincter.
2. Urge Incontinence
- Causes: (1) Cystitis; (2) Hyperactive neurogenic bladder.
- Pathogenesis: Detrusor irritability and hyperactivity are present. The patient feels urgency in the presence of small amounts of urine in the bladder. Urine escapes if the intravesical pressure exceeds the maximum urethral pressure before the patient is able to reach the bathroom.
- Urodynamics: Involuntary detrusor contractions (detrusor contractions occur normally during micturition only) with normal maximum urethral pressure.
- Treatment: Treat the cause.
3. Sphincteric Incontinence
- Causes: (1) Severe urethral injury: (2) latrogenic after TURP.
- Diagnosis by urodynamics: Loss of internal and external urethral sphincter activities.
- Treatment: Surgical placement of an artificial urethral sphincter.
4. Overflow Incontinence
Review chapter: Retention of Urine.
5. Nocturnal Enuresis
Definition: Bed wetting in children beyond the age of 3 years.
Causes: Not clearly known. However, enuresis is frequently associated with 1 one of the following features: hyperactive detrusor contractions (diagnosed by cystometry); nocturnal polyuria, and psychogenic disturbances.
Treatment: Based on the associated findings:
- Hyperactive detrusor contractions: give Imipramine (Tofranil) tablets (25-75 mg once daily before bedtime): it has an anticholinergic effect that reduces intravesical pressure. Hyperactive detrusor contractions are sometimes 2ry to congenital urethral meatal stenosis. Surgical widening of the urethral meatus by meatotomy usually cures the enuresis without the need for medications.
- Nocturnal polyuria: restrict fluid intake at least 2 hours before bedtime, and encourage the child to empty the bladder immediately before sleeping. Also, give Desmopressin (an antidiuretic that reduces the volume of urine output during sleep). It is given as a (nasal spray with a 70% success rate.
- Psychogenic disturbances: Psychotherapy with strict instructions to the parents not to punish their child for wetting the bed.
6. Congenital Incontinence
- Causes: (1) Ectopia vesicae (bladder exstrophy; (2) Complete epispadias.
- Treatment: Treat the cause.
7. Fistulous Incontinence
A) Uretero-vaginal fistula:
- Cause: latrogenic injury of the ureter and vagina with compromised blood supply during a difficult pelvic operation. Ischemia and necrosis occur in the walls of the ureter and vagina, and a fistula develops a few days later.
- Presentation: Urine leak from the vagina (urine passing through the fistula leaks from the vagina while urine from the other ureter passes normally to the bladder, and is voided in a normal way) + Renal pain from ureteral stricture at the site of the fistula causing hydroureter and hydronephrosis.
- Treatment: Excision of the fistula, and surgical reconstruction of the ureter at least 3 months after the injury when the wound has healed completely.
B) Vesico-yaginal fistula:
- Cause: Iatrogenic injury of the bladder and vagina with compromised blood supply during a difficult pelvic operation. Ischemia and necrosis occur in the walls of the bladder and vagina, and a fistula develops a few days later.
- Presentation: Complete leak of urine (all bladder urine passing through the fistula leaks from the vagina). A big fistula is easily palpated by vaginal examination, and the definitive diagnosis is by cystoscopy.
- Treatment: Excision of the fistula, and surgical reconstruction of the bladder, at least 3 months after the injury when the wound has healed completely.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
What are urinary tract infections?, kidney problems, Urinary retention, and Bladder stones
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid and protein metabolism
Histological structure of kidneys, Uriniferous tubules, and Types of nephrons
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption and secretion
Urinary passages function, structure of Ureter, Urinary bladder, and Uvulae vesicae
Urinary system structure, function, anatomy, organs, Blood supply, and Importance of renal fascia
Urinary bladder structure, function, Control of micturition by Brain, and Voluntary micturition