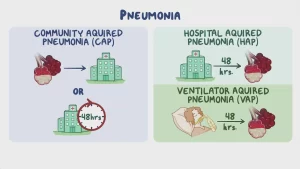
Hospital Acquired Pneumonia symptoms and treatment, What is the difference between HAP and VAP?
Hospital-acquired pneumonia is often serious because the bacteria causing it are more resistant to antibiotics and because the people who get it are already sick. Patients put on ventilators, often in intensive care units, can get ventilator-associated pneumonia (VAP).
Hospital Acquired Pneumonia
Hospital-acquired pneumonia (HAP) is a serious lung infection that occurs in people during a hospital stay, typically at least 48 hours after being admitted. It is a common healthcare-associated infection (HAI) and can lead to significant morbidity and mortality.
Common organisms include:
- Gram-negative bacilli like Escherichia coli, Klebsiella spp., Pseudomonas, Acinetobacter, and Enterobacter among others usually multidrug-resistant.
- Gram-positive cocci like Staphylococcus aureus; are both Methicillin-sensitive and resistant. although the latter is more prevalent.
- Other viruses and fungi that are more prevalent in immunocompromised and severely ill patients.
Clinical manifestations of pneumonia may include:
- Fever, sweating, and shaking chills (Hypothermia can occur in extremes of age and immune-compromised patients).
- Cough (productive).
- Dyspnea, tachypnea, and tachycardia.
- Chest pain on breathing or coughing.
- Nausea, vomiting, or diarrhea especially at a young age.
High-risk groups of people:
- Elderly above 65 years.
- Children under 2 years.
- People with an underlying health condition especially asthma, chronic obstructive pulmonary disease (COPD), or heart disease.
- People with weakened immune systems e.g. hospitalized patients, people who have HIV/AIDS, organ transplant, or who receive chemotherapy or long-term steroids are at risk.
- Habits, such as smoking, heavy alcohol use, and malnourishment which suppress the immune system.
Complications
- Even with treatment, some people with pneumonia, especially those in high-risk groups, may experience complications, including:
- Bacteremia, spreading the infection to other organs, potentially causing meningitis or organ failure.
- Pleural effusion and empyema.
- Lung adhesions, fibrosis & abscess.
Diagnosis
Sometimes pneumonia can be difficult to diagnose because the symptoms are so variable and are often very similar to those seen in a cold or influenza.
- History of exposure: Any recent travel, occupation, contact with animals, exposure to other sick people at home, recent illnesses
- Physical examination: refer to signs and symptoms.
- Laboratory Diagnosis: Routine Blood tests: includes CBC with differential count, ESR, CRP, and Procalcitonin.
- Microbiological examination: Specimens may include (ideally before antibiotics):
- Sputum (either expected or ated or induced).
- Lower respiratory tract (LRT) specimens were collected using a bronchoscope; bronchoalveolar lavage (BAL) or mini-BAL.
- Blood: for blood culture as bacteremia is present in about 1/3 of pneumonia cases.
- Pleural fluid in case of pleural effusion for analysis and culture.
A) Microscopic examination of sputum: Gram-stained smear: presumptive diagnosis can be done in the presence of pus cells with putative pathogen e.g predominant gram-positive diplococci suggests pneumococcal pneumonia. Zeihl Neelsen stain: For detection of acid fast bacilli (TB).
B) Bacterial culture and antimicrobial susceptibility testing will allow the growth of Pneumococci, H. influenzae, Staphylococci and gram-negative bacilli.
C) Rapid antigen detection for pneumococcal and legionella from sputum and urine.
D) Multiplex PCR tests for diagnosis of atypical bacterial and viral pneumonia are available. These tests are rapid, sensitive and specific.
E) Serological tests using ELISA, immunofluorescence or latex agglutination can detect IgM antibodies or a rising titer suggestive of recent active infection, especially in viral pneumonia.
F) Fungal culture can be done from LRT specimens to detect Candida spp., Aspergillus spp. and Cryptococcus.
Pneumocystis are detected either by immunofluorescence or PCR from LRT specimens. Elevated Beta-glucan in serum indicates fungal infection.
5) Radiology: Chest X-ray detects opacity of the chest (lobar consolidation in case of bacterial pneumonia and interstitial pneumonitis in viral cases).
6) In high-risk patients some additional tests, including:
- CT scan of the chest.
- Pulse oximetry or more precisely arterial blood gas test to measure the oxygen level.
- Bronchoscopy, Fluid samples, or a biopsy of lung tissue can be taken from the lower respiratory tract.
Prevention
1) Vaccination:
- Viral vaccines are available for influenza virus and SARS-CoV-2 (COVID-19).
- Bacterial vaccines are available for Pneumococci and Hib.
1. Pneumococcal vaccines
Currently, there are two types. They are given by injection and are generally safe.
Polyvalent vaccine (Pnemovax)
- Prepared from polysaccharide capsules of 23 serotypes.
- Susceptible groups older than 2 years, e.g., diabetics, chronic pulmonary disease, immunocompromised, elderly patients.
Pneumococcal polysaccharide conjugate vaccine (Prevenar 13)
- It contains 13 pneumococcal antigens conjugated to a protein to stimulate the immune response.
- Effective in infants and children below 2 years.
2. Haemophilus b conjugate vaccine
- It is formed of polysaccharide conjugated to a protein carrier (The protein conjugate used is either the tetanus toxoid or the outer membrane protein complex of Neisseria meningitidis serogroup B).
- It is given as a part of PENTA valent (DPT, HBV, Hib) compulsory vaccination of infants in Egypt at 2,4,6 months.
2) Avoid overcrowding and allow better ventilation.
3) Good hygiene practices. Washing hands regularly, use an alcohol-based hand sanitizer, and cough etiquette.
4) Avoid close contact with animals.
5) Stop smoking, alcohol abuse, and addiction. Which damages the lungs‘ natural defenses against respiratory infections.
6) Healthy lifestyle. Enough rest and sleep, regular exercise, a healthy diet, and good hydration.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Pneumonia causes, types, treatment, Is pneumonia usually serious? and Is pneumonia contagious?
Chronic Obstructive Pulmonary Diseases Treatment, Types and Causes of COPD
Steps of Asthma control, What is good control of asthma? and What is asthma management?
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax