Hospital-Acquired Pneumonia (HAP) treatment, What is the most common cause of HAP?
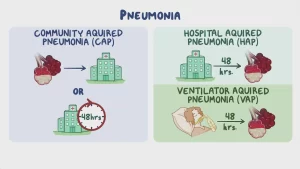
Hospital-acquired pneumonia (HAP) (Nosocomial Pneumonia) is a type of pneumonia that develops 48 hours or more after hospital admission and is not present or incubating at the time of admission, It is a serious healthcare-associated infection with significant morbidity, mortality, and healthcare costs.
Hospital-Acquired Pneumonia (HAP)
HAP: is pneumonia that occurs 48 hours or more after admission and does not appear to be incubating at the time of admission.
Ventilator-associated pneumonia (VAP:) is a subtype of HAP that develops more than 48-72 hours after endotracheal intubation.
Healthcare-associated pneumonia (HCAP): Any patient who:
- Hospitalized in an acute care hospital for two or more days within the last 90 days.
- Resided in a nursing home or long-term care facility.
- Received recent IV antibiotics, chemotherapy, or wound care within the past 30 days.
Incidence
- 13-1.8% of Nosocomial infection.
- 10-25% of ICU patients.
- Mortality up to 70%.
Nosocomial Pneumonia
Pathogens
- G-ve bacilli (60%): Pseudomonas aeruginosa, Klebsiella, Proteus, E. coli, Hemophilus influenzae, Moraxella catarrhalis.
- G+ve cocci (20-40%): Staphylococcus aureus, Streptococcus pneumoniae.
- Anaerobic bacteria, Mycobacterium tuberculosis, viruses, fungi or protozoa.
Pathogenesis
- Bacterial colonization of the aerodigestive tract by gram-negative enteric bacteria (core organism) and aspiration of the contaminated secretions into the normally sterile lower respiratory tract within the first 5 days (early onset).
- Cross-transmission between patients through healthcare personnel (late-onset i.e., after 5 days).
Diagnosis of nosocomial pneumonia
- Alveolar infiltrates on chest X-ray + 2 or more of the following: Hypo/hyperthermia (<36 or > 38 °C). Leucopenia or leukocytosis. Purulent tracheal secretions. Decreased PaO2.
- Qualitative and quantitative culture of lower airway secretions.
- blood culture which is mandatory (Low sensitivity + specificity).
- Quantitative culture using invasive methods (PSB+BAL): PSB: Protected specimen brush, BAL: Broncho-Alveolar lavage.
Diagnosis of ventilator-associated pneumonia (VAP)
New and persistent X-ray infiltrates + one of the following:
- Positive culture of pleura, blood, or tracheal aspirates.
- X-ray cavitations.
- Histopathologic evidence.
- New fever and leukocytosis.
Risk Factors
- Recent abdominal surgery.
- Witnessed aspiration.
- D.M.
- Prolonged ICU stay.
- Coma.
- Corticosteroids.
- Head trauma.
- Prior antibiotics.
- Renal failure.
- Structure lung disease.
Onset
- Early before 5 days.
- Late on or after 5 days.
Sever Pneumonia = ICU
- Respiratory rate > 35/min.
- Hypoxemia.
- There is a need for M. V.
- Rapid X-ray worsening.
- Shock.
- Oligure.
- Renal failure.
Risk Factors for Multidrug-Resistant Pathogens
Risk factors for MDR VAP
- Prior intravenous antibiotic use within 90 d.
- Septic shock at the time of VAP.
- ARDS preceding VAP.
- Five or more days of hospitalization before the occurrence of VAP.
- Acute renal replacement therapy prior to VAP onset.
Risk factors for MDR HAP
Prior intravenous antibiotic use within 90 d.
Risk factors for MRSA VAP/HAP
Prior intravenous antibiotic use within 90 d.
Risk factors for MDR Pseudomonas VAP/HAP
Prior intravenous antibiotic use within 90 d.
Treatment
Recommended Initial Empiric Antibiotic Therapy for Hospital-Acquired Pneumonia (HAP) (Non- Ventilator-Associated Pneumonia)
1. Category I: (Monotherapy)
Not at high risk of mortality or drug resistance→ Choose one antibiotic from the following groups:
- Antipseudomonal cephalosporin e.g., Cefepime or Ceftazidime.
- Carbapenems e.g., Imipenem or Meropenem.
- Antipseudomonal fluoroquinolone e.g., Levofloxacin or Ciprofloxacin.
If associated factors Increase the likelihood of MRSA → add anti-MRSA e.g. Linezolid or Vancomycin, Teicoplanin (Most common used in Egypt).
2. Category II: (Triple therapy)
High risk of mortality or receipt of intravenous antibiotics during the prior 90 days: Give Double antipseudomonal + anti-MRSA (Linezolid or Vancomycin).
- The first antipseudomonal should be an antipseudomonal cephalosporin (Cefepime or Ceftazidime) or an antipseudomonal penicillin (Piperacillin- tazobactam) or a carbapenem (imipenem or Meropenem).
- The second antipseudomonal should be an antipseudomonal fluoroquinolone (Levofloxacin or Ciprofloxacin) or an aminoglycoside (Amikacin or Gentamycin).
- Empirical anti-MRSA: (Linezolid or Vancomycin).
Recommended Initial Empiric Antibiotic Therapy for Ventilator-Associated Pneumonia (VAP)
Same treatment as category II in HAP (Double antipseudomonal + Anti MRSA)
- Antipseudomonal cephalosporin eg. Cefepime or ceftazidime.
- Or Antipseudomonal penicillins eg Piperacillin-tazobactam.
- Or Carbapenems eg Imipenem or Meropenem.
Plus
- Antipseudomonal flouroquinolone eg. Levofloxacin, ciprofloxacin.
- OR Aminoglycoside eg. Amikacin, gentamycin.
- OR Polymyxins eg. Colistin or Polymyxin B.
Plus
Anti-MRSA: Linezolid OR Vancomycin.
Assessment of Non-Responders
Wrong diagnosis
- Atelectasis.
- Pulmonary embolism.
- ARDS.
- Pulmonary hemorrhage.
- Underlying disease.
- Neoplasm.
Nebulizer or Inhaler to avoid systemic toxicity of Certain drugs if they are given together. e.g. Fluoroquinolones, Aminoglycosides (Amikacin & Gentamicin; Combination of both causes Nephropathy)
Wrong organism
- Drug-resistant pathogen (bacteria, mycobacteria, virus, fungi).
- Inadequate antimicrobial therapy.
Complications
- Empyema.
- Lung abscess.
- Clostridium defficile colitis.
- Occult infection.
- Drug fever.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Inflammation of the lung parenchyma, What causes lung parenchyma?, Is lung parenchyma dangerous
Hospital-Acquired Pneumonia symptoms and treatment, What is the difference between HAP and VAP?
Pneumonia causes, types, treatment, Is pneumonia usually serious? and Is pneumonia contagious?
Chronic Obstructive Pulmonary Diseases Treatment, Types and Causes of COPD
Steps of Asthma control, What is good control of asthma? and What is asthma management?
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax