Histology of pancreas, Structure of islets of Langerhans, Insulin function and Metabolism
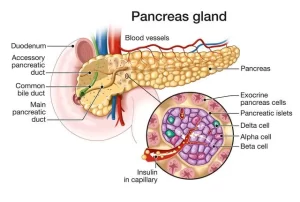
The pancreas is located inside the abdomen, just behind your stomach, It is about the size of your hand, the pancreas helps the digestive system by making hormones, It has exocrine glands that produce enzymes important to digestion, These enzymes include trypsin & chymotrypsin to digest proteins; amylase for the digestion of carbohydrates; and lipase to break down fats.
Histology of the pancreas
The pancreas is one of the largest accessory glands of the digestive tube. It lies in the abdominal cavity occupying the duodenal cap. The secretory parenchyma is peculiar in that it is composed of both endocrine and exocrine parts and therefore it is classified as a mixed gland.
The endocrine parenchyma of the pancreas (The islets of Langerhans)
The islets of Langerhans are generally more numerous in the tail region than in the head and body of the pancreas.
Histological structure of the islets of Langerhans
A. The stroma: islets appear in routine histological sections, as lightly-stained areas of variable sizes between the pancreatic acini. They are not encapsulated but supported by delicate reticular fibers.
B. The parenchyma: The cells of the islets are polygonal, arranged in short cords, and separated by a rich network of fenestrated capillaries. By histochemical and immunohistochemical staining of sections of the pancreas, at least 3 main types of cells in pancreatic islets can be identified. They include:
1. A (α) cells
These cells are larger but less numerous than the B cells (20%). They usually occupy the periphery of the islet. By EM, their secretory granules are numerous and have a homogeneous dense core. Function: secretion of the glucagon hormone.
2. B (β) cells
They are small cells constituting the majority (70%) of the islet cells. They usually occupy the central zone of the islet. By EM, their secretory granules have a characteristic polyhedral crystalline dense core surrounded by a wide electron-lucent halo.
Functions of β cells
- Release of insulin.
- β cells release C-peptide, a consequence of insulin production, into the bloodstream, C-peptide helps to prevent neuropathy and other symptoms of diabetes related to vascular deterioration, Measuring the levels of C-peptide can give a practitioner an idea of the viable beta-cell mass.
- GABA (y amino butyric acid) is produced by the pancreatic beta-cell, GABA released from beta cells can act on GABA A receptor in the α cells, causing membrane hyperpolarization and hence suppressing glucagon secretion
3.D (δ) cells
They constitute about 5-10% of the islet cells. They are, like the A cells, peripherally located in the islet. Function: secretion of somatostatin hormone.
Insulin
Insulin is a polypeptide consisting of 2 chains A and B linked by 2 interchaindisulphide bridges that connect A7 to B7 and A20 to B19. A third intrachain disulfide bridge connects residues 6 and 11 of the A chain, The A chain is composed of 21 amino acids while the B chain is composed of 30 amino acids.
Metabolism of insulin
Insulin has no plasma carrier protein, thus its plasma half-life is less than 3-5 minutes, The major organs involved in insulin metabolism are the liver, kidneys, and placenta, About 50% of insulin is removed in a single pass through the liver.
The metabolism of insulin molecules involves 2 enzyme systems:
The first involves an insulin-specific protease found in many tissues especially the liver, and kidneys, thus the insulin molecule could be cleaved proteolytically between amino acid residues 16 and 17 of the B chain.
The second mechanism involves hepatic glutathione-insulin transhydrogenase. This enzyme reduces the disulfide bonds, and then the individual A and B chains are rapidly degraded.
Mechanism of insulin action
Some receptors have intrinsic tyrosine kinase activity that is activated by binding of the specific hormone resulting in the phosphorylation of protein substrates on tyrosine residues. The activated tyrosine kinase can initiate a phosphorylation and dephosphorylation cascade in the cell.
The insulin receptor is a glycoprotein. It has 2 identical α chains and two transmembrane β subunits linked together (α2β2) by disulfide bonds. The α chains contain the insulin binding domain, β chains have a tyrosine kinase domain and an autophorylations site. The phosphorylated receptor next phosphorylates insulin receptor substrates (IRS). IRS1 is involved in the cell growth effects of insulin (slow action of insulin).
Activation of IRS1 activates several proteins, a pathway that ends by activation of MAP kinase (mitogen-activated protein kinase) which stimulates cell growth and DNA synthesis. IRS2 is involved in the metabolic effects of insulin (rapid action of insulin). The phosphorylated IRS2 binds to a variety of proteins:
One of these proteins is Pl-3 kinase links activated insulin receptors to a Protein 70 kinase. This pathway is involved in the translocation of glucose transporter from Golgi apparatus to the cell membrane to bind glucose, enzyme activities (dephosphorylation and activation of glycogen synthase) and regulation of genes involved in metabolism e.g, increase of glucokinase synthesis and inhibition of PEPCK synthesis.
Elevated blood insulin levels, such as in obesity or insulinoma, down-regulate concentration of insulin receptors, With low insulin concentrations, the number of receptors increases (up-regulation) and responsiveness to insulin increases e.g. obese type II diabetics may recover by increasing insulin responsiveness as a result of dieting.
Functions of insulin
a) Effect of insulin on carbohydrate metabolism
- Insulin facilitates glycogen synthesis in the liver by increasing the activity of enzymes required for the formation of glycogen.
- Insulin inhibits gluconeogenesis by decreasing the quantities and it activities of the liver enzymes required for gluconeogenesis.
- Insulin inhibits glycogenolysis, the breakdown of glycogen into glucose.
- Insulin facilitates the entry of glucose into the cells (muscles, adipose tissues, and connective issues by an action on the cell membrane, The normal resting muscle membrane is almost impermeable to glucose except when the muscle fiber is stimulated by insulin.
- During periods of heavy exercise, exercising muscle fibers become highly permeable to glucose even in the absence of insulin because of the contraction process itself.
- The brain cells are permeable to glucose without the intermediation of insulin, except for the satiety center.
b) Effect of insulin on fat metabolism
Insulin exerts multiple effects to lower blood fatty acids & promote triglyceride storage:
- Insulin increases the utilization of glucose which automatically decreases the utilization of fat, thus functioning as a “fat sparer”.
- Insulin also promotes lipogenesis in the cells and adipose tissue.
- It promotes chemical reactions that use fatty acids and glucose derivatives for triglyceride synthesis.
- It inhibits lipolysis (fat breakdown), reducing the release of fatty acids from adipose tissue into the blood.
c) Effect of insulin on protein metabolism
Insulin lowers blood amino acid levels and enhances protein synthesis through several effects:
- Insulin causes the active transport of many of the amino acids into the cells.
- Insulin offers a direct effect on the ribosomes to increase the translation of ger RNA, forming new proteins.
- Insulin also inhibits the catabolism of proteins.
- In the liver, insulin depresses the rate of gluconeogenesis, This conserves the amino acids in the protein stores of the body.
d) Effect of insulin on growth
Insulin has a synergistic effect with growth hormone, Each promotes cellular uptake of a different selection of amino acids, all of which are required for growth.
e) Effect of insulin on potassium
It causes K+ to enter muscle cells. The reason is that insulin increases the activity of Na+– K+ ATPase in the cell membrane, so more potassium ion is pumped into the cell.
PI-3kinase (phosphatidyl inositol-3kinase) is a protein containing 2 subunits: one unit interacts with activated insulin receptor substrates, the other subunit phosphorylates (activates) other proteins like P70 kinase and mediates the different metabolic functions of insulin.
You can subscribe to Science Online on YouTube from this link: Science Online
Cortisol effects, Cause of melanin deposition, Adrenal androgens, and Adrenogenital Syndrome
Glucocorticoid (cortisol) function, Effects of cortisol on skeletal muscle and circulatory system
Calcium metabolism, Calcitonin function, Vitamin D3 & Biosynthesis of calcitriol
Parathyroid gland anatomy, structure, function, hormones and Tetany types
Endocrine system structure, function, disorders, Endocrine Glands and Hormones types