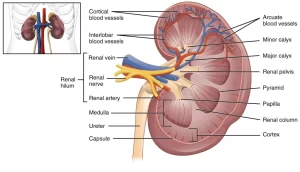
Histological structure of kidneys, Uriniferous tubules and Types of nephrons
The kidneys are paired, bean-shaped organs located on either side of the spine, just below the rib cage. They filter waste and excess substances from the blood to form urine. They regulate electrolytes, fluid balance, and acid-base balance. They produce hormones like erythropoietin and renin, They eliminate waste products like urea, creatinine, and drugs.
Uriniferous tubule
The renal parenchyma represents a compound tubular gland as each kidney is formed of about 1- 4 million uriniferous tubules (structural unit of the kidney). The renal tubules are held together by the renal interstitium, where a delicate network of reticular fibers supporting the parenchymal elements, blood vessels, and interstitial fibroblasts are present. The uriniferous tubule is formed of 2 parts with a different embryological origin, these are:
A. The nephron: is composed of:
- Renal corpuscle.
- Proximal convoluted tubule (PCT).
- Loop of Henle.
- Distal convoluted tubule (DCT).
- A short connecting tubule links the nephron to.
B. The collecting duct.
Longitudinal hemi-section of the kidney shows
- Each kidney has a concave medial border, the hilum through which the renal vessels and nerves pass, and the funnel-shaped expanded origin of the ureter, the renal pelvis exits. The renal pelvis originates from 2 or 3 major calyces, which are further originating from smaller minor calyces.
- The renal tissue is differentiated into:
- The cortex: the darker outer layer with a granular appearance due to the presence of the highly vascular renal corpuscles and the convoluted renal tubules.
- The medulla: the paler inner layer with striated appearance due to the longitudinally organized straight renal tubules and collecting ducts together with their surrounding vasculature. The medulla, in human is composed of 8-12 renal pyramids. Their bases form the corticomedullary junction. Their apices, the renal papillae, protrude into the minor calyces. The tip of the papilla is perforated by the openings of the collecting ducts and hence called the area cribrosa.
- The medullary rays: these are striations extending from the medulla into the cortex representing the straight segments of renal tubules and the cortical collecting ducts.
Types of nephrons
According to the position of the renal corpuscles in the cortex, nephrons are classified into:
- Subcapsular nephrons (short-looped nephrons), with their renal corpuscles lying under the capsule, They have very short loops of Henle.
- Juxtamedullary nephrons (long-looped nephrons).
- Intermediate nephrons, with loops of Henle of intermediate lengths.
Intrarenal vasculature
The renal artery, on entering the renal hilum divides into many interlobar arteries that run between the renal pyramids. At the corticomedullary junction, these arteries turn to follow an arched course along with the bases of the pyramids forming the arcuate arteries. From the arcuate arteries, interlobular arteries branch off at right angles. They ascend through the cortex and give off the afferent arterioles, to the nearby renal corpuscles.
Each afferent arteriole divides into a first capillary network, the glomerular capillaries which unite to form the efferent arteriole, which divides into a second capillary network. Being situated between two capillary beds, the efferent arteriole is considered as an arterial portal circulation. The arrangement of the second capillary network differs according to the position of the renal corpuscle from which they originate:
- In the subcapsular and intermediate corpuscles, efferent arterioles give rise to the fenestrated peritubular cortical capillaries that surround the nearby renal tubules.
- In the juxtamedullary corpuscles, efferent arterioles give rise to the vasa recta. These are thin, straight capillary loops that run close and parallel to the descending and ascending limbs of the loop of Henle and the collecting ducts.
The venous drainage follows the same course as the corresponding arteries, the venous ascending limbs of vasa recta drain into the arcuate veins. The difference in color between the cortex and medulla reflects the distribution of intrarenal vasculature (90-95% of blood passes through the cortex and only 5-10% passes through the medulla).
Physiological characteristics of renal circulation
Almost all renal blood has to pass through the glomeruli. Renal circulation is portal circulation. blood circulates into two capillary networks: the glomerulus and the peritubular capillaries. The glomerular capillaries are the only capillaries in the body that drain into arterioles. The efferent glomerular arteriole is a portal artery. The portal renal system has 2 functions.
- Filtration through the glomerular capillaries.
- Reabsorption and secretion through the peritubular capillaries.
The kidneys have a high blood flow rate. One-fourth of the cardiac output passes into the kidney/minute (1300 ml blood/minute). The high renal blood flow does not reflect a high O2 consumption, kidneys utilize 8% of the total O2 consumption of the body.
This high blood flow is related to the homeostatic function of the kidney which allows a high rate of glomerular filtration, out of 700 ml of plasma flowing through the glomeruli 120 ml are filtered into the capsule; 99% of the filtrate is reabsorbed by the renal tubules leaving behind unwanted substances to be excreted in the urine.
Pressures in the renal circulation
The two major areas of resistance to blood flow in the nephron are the afferent and the efferent arterioles. In the afferent arteriole, the pressure falls from 100 mmHg at its arterial end to a mean pressure of about 60 mmHg in the glomerulus.
As the blood flows through the efferent arterioles from the glomerulus to the peritubular capillary system, the pressure falls another 47 mmHg to a mean peritubular capillary pressure of about 13 mmHg. Thus, the high-pressure capillary bed in the glomerulus, acts at a mean pressure of about 60 mmHg causes rapid filtration of fluid into the Bowman’s capsule.
On the other hand, the low-pressure capillary bed in the peritubular capillary system acts at a mean capillary pressure of about 13 mmHg which allows rapid absorption of fluid because of the high osmotic pressure of plasma.
Histological structure of the nephron
1. Histological structure of the renal (Malpighian) corpuscle
The renal corpuscle is a rounded structure situated in the renal cortex. Each renal corpuscle has two poles:
- Vascular pole, where an afferent arteriole enters the glomerulus and efferent arteriole leaves.
- Urinary pole, where the proximal convoluted tubule begins.
Components of the renal corpuscle
a. The Bowman’s capsule: is made up of:
- Parietal layer, of simple squamous epithelium. At the urinary pole, the epithelium changes abruptly to the simple cuboidal epithelium lining the proximal convoluted tubule.
- Bowman’s space (urinary space), which is the space between the two layers of Bowman’s capsule. It receives the fluid filtered from the glomerular capillaries. At the urinary pole, this space is continuous with the lumen of the proximal convoluted tubule.
- Visceral layer, which covers the glomerular capillaries formed by the podocytes (modified epithelial cells). Podocytes are large stellate cells with 2 types of cytoplasmic processes:
- Primary processes arise from the cell body and are separated from the underlying glomerular capillaries by the narrow subpodocytic space which is a part of the Bowman’s space.
- Secondary processes (foot processes) or (pedicels), which arise from each primary process. They are adherent to the glomerular capillary and interdigitate with the secondary processes of adjacent podocytes forming the filtration slits, through which the glomerular filtrate can enter into the Bowman’s space. These slits are bridged by slit diaphragms, which are formed of the glycocalyx of the adjacent pedicels.
b. The glomerulus: on entering the renal corpuscle the afferent arteriole divides into a tuft of fenestrated glomerular capillary lobes, invaginated into the Bowman’s capsule.
c. The mesangium: it is the connective tissue filling the interstitial spaces between the glomerular capillaries at the surfaces that are not covered by the podocytes. It consists mainly of the intraglomerular mesangial cells, which are pericyte-like cells with cytoplasmic processes. The mesangial cells support the glomerular capillary walls where podocytes are lacking. They are also responsible for the continuous turnover of the glomerular basement membrane by phagocytosis of the filtration residues while its renewal is done by the podocytes and the glomerular endothelial cells.
Filtration barrier of the kidney
It is the barrier formed by components of the renal corpuscle for formation of an ultrafiltrate containing unwanted waste products and conserving the valuable molecules in plasma. Therefore, filtration occurs through the following structures:
- The fenestrated endothelium of glomerular capillaries: forms an initial physical barrier to the passage of blood elements (RBCs, leukocytes, platelets) from the capillary lumen to the Bowman’s space.
- The glomerular basement membrane: it is the common fused basal lamina of the glomerular capillary endothelial cells and the podocytes. It is the principal component of the filtration barrier.
- The filtration slit diaphragms: it restricts the filtration of the small proteins.
2. Histological structure of the renal tubules
A. Proximal convoluted renal tubules (PCT)
The PCT begins abruptly at the urinary pole of Bowman’s capsule, This part is responsible for the obligatory reabsorption of most of the glomerular filtrate.
Histological features of the proximal convoluted tubules
- Being the longest convoluted segment of the nephron (14mm long) with a large diameter (60 μm), their cut sections are frequently seen in the histological section, particularly near the renal corpuscles in the cortex.
- In cross-section, PCT appears rounded and lined by large pyramidal cells with spherical nuclei situated nearer to the base.
- The lining cells exhibit histological features of reabsorption and active ion transport: The lumen is narrow and almost occluded due to a well-developed brush border (long, numerous microvilli) with apical endocytotic vesicles. They have deep eosinophilic cytoplasm with indistinct lateral cell boundaries and basal striations (abundant mitochondria with basolateral-infolded cell membrane).
B. Loop of Henle
The loop of Henle plays a key role, in coordination with the vasa recta and renal interstitium in the medulla, for the mechanism of urine concentration. The loop of Henle has four segments that differ in their lining epithelium and the degree of permeability to water, salts, and urea. These are:
1. The thick descending limb: it is a straight continuation of the proximal convoluted tubule to enter the medulla with a lining epithelium nearly similar to that of proximal convoluted tubules.
2. & 3. The thin descending and the thin ascending limbs: take a U-shaped course in the medulla and are lined by simple squamous epithelium with few organelles.
4. The thick ascending limb: this segment is the straight part of the distal convoluted tubule with its lining epithelium. It enters the cortex, running in the medullary ray, where it comes in close contact with the vascular pole of the renal corpuscle of its own nephron to form the macula densa of the juxtaglomerular apparatus, and then it becomes the distal convoluted tubule.
C. Distal convoluted renal tubules (DCT)
The thick ascending limb of the loop of Henle enters the cortex to mark the beginning of the DCT. This segment is responsible for facultative reabsorption of water and electrolytes (aldosterone-dependent) and shares in the acidification of urine.
Histological features of the distal convoluted tubules
- Compared to the PCT, the distal tubules are shorter (5mm long) with a smaller diameter (20-25 um) so their cut sections are less frequently seen in the cortex.
- In cross-section, they are lined by short cuboidal cells with spherical nuclei, situated nearer to the apex.
- The lining cells exhibit histological features of active ion transport: The lumen is relatively wide with no brush border (few, short microvilli associated with few endocytotic vesicles). They have pale eosinophilic cytoplasm with more distinct intercellular boundaries and prominent basal striations (less abundant mitochondria but extensive deep basal membrane in foldings that tend to push the nucleus apically).
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia
Suprarenal glands (adrenal glands) anatomy, structure & Effect of Deficiency of Catecholamines
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Functions of the loop of Henle, distal tubules, collecting ducts & Glucose tubular maximum