Histological organization of pharynx, Structure and function of esophagus
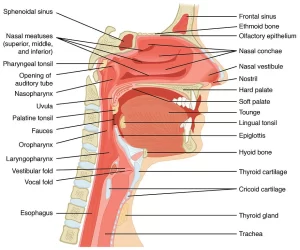
The pharynx is a musculo-membranous tube that extends behind the nasal cavities, the mouth, and the larynx. The mucous membrane of the pharynx differs in its lining epithelium from one part to the other.
Histological organization of pharynx
Accordingly, Pharynx is divided into:
- The nasopharynx, lined by the respiratory epithelium, pseudostratified ciliated columnar epithelium with goblet cells.
- The oropharynx, is a common passage for air and food lined by non-keratinized stratified squamous epithelium.
- The laryngopharynx (hypopharynx), is lined by non-keratinized stratified squamous epithelium.
The lamina propria contains seromucous glands and is formed of dense fibroelastic connective tissue separating the epithelium from the striated muscles of the pharynx.
General histological plan of the alimentary canal
On cross-section, the wall of the gut is formed of four basic histological layers. From the lumen outward, they are:
Muscosa also called the mucous membrane
It is the most variable layer, composed of:
- The surface epithelium shows regional variations to serve the specific function of each segment of the gastrointestinal tube.
- The lamina propria: a layer of loose connective tissue rich in blood and lymph vessels, It may also contain glands and lymphoid tissue.
- The muscularis mucosae: is a thin layer of smooth muscle fibers usually arranged in an inner circular and an outer longitudinal direction, It separates the mucosa from the submucosa. Muscularis mucosae promotes movement of the mucosa, independently from the other movements of the digestive tract, thus increasing its contact with food.
Submucosa
It is a layer of dense fibro-elastic connective tissue rich in blood and lymph vessels. It contains the submucosal autonomic nerve plexus (Meissner’s plexus). It may also contain glands and lymphoid tissue. The lymphoid tissue in the lamina propria and submucosa of the gut constitutes a part of MALT (mucosa-associated lymphoid tissue) that provides protection against bacterial invasion since most of the digestive tract is lined by a thin epithelium (except the oral cavity, esophagus, and anal canal).
Musculosa
It is also called Muscularis externa, it consists of Spirally-arranged smooth muscle fibers that are usually organized in an inner circular layer and an outer longitudinal layer. Musculosa creates a series of peristaltic waves which move the food within the lumen of the gut. The myenteric autonomic nerve plexus (Auerbach’s plexus) is situated in the thin connective tissue found in between the two layers of the smooth muscle fibers.
Serosa
A thin layer composed of: Loose connective tissue traversed by large blood and lymph vessels and nerve trunks. Sometimes contains a large amount of adipose tissue. The mesothelial covering of simple squamous epithelium (visceral peritoneum). Serosa provides a smooth surface covering the viscera to facilitate their free movement. When the peritoneum is not covering the viscus, this layer is called Aventitia (Fibrosa) which protects the viscera and fixes them to the thoracic, abdominal, and pelvic walls.
The histological structure of esophagus
The esophagus is a muscular organ responsible for the transport of the masticated food bolus from the mouth down to the stomach. Its greatest part lies in the thorax except for the terminal ½ inch which passes through the diaphragm to lie in the abdominal cavity.
Histological structure of T.S of the esophageal wall
Mucosa
1- The surface epithelium: non-keratinized stratified squamous epithelium which is suitable in this site as:
- It allows the esophageal mucosa to resist friction by the rough ingested food bolus as it goes down the esophageal tube.
- It is subjected to continuous renewal by mitosis of the basal cell layer.
2- The lamina propria: formed of:
Loose connective tissue rich in blood vessels, nerves, and lymphatics.
The mucosal esophageal glands that are:
- Present near the junction with the stomach and similar to the cardiac glands of the gastric mucosa.
- Secreting neutral mucus. This secretion, in combination with that of the cardiac glands, protects esophageal mucosa against regurgitated stomach contents.
3- The muscular is mucosae: represented by scattered bundles of longitudinal smooth-muscle fibers. In the lower part of the esophagus, this layer becomes more differentiated into inner circular and outer longitudinal smooth muscle layers.
Submucosa
Dense fibro-elastic connective tissue contains the submucosal esophageal glands that are:
- Found along the entire esophageal length. Formed of groups of mucous acini with their ducts open on the luminal surface.
- Secreting mucus to lubricate the mucosa.
Musculosa
It is arranged in inner circular and outer longitudinal muscle layers. In the upper third of the esophagus, it is formed of striated muscle fibers, in the middle third; it is formed of a mixture of both striated and smooth muscles, while in the lower third it is made up of smooth muscle fibers only.
Adventitia
It is formed of loose areolar connective tissue, The abdominal part of esophagus is covered by Serosa.
Physiology of the esophagus
The oesophagus is a muscular tube about 25cm long.
Function of the esophagus
The normal oesophagus has two main functions; a transfer function and an anti-reflux function. By virtue of the transfer function, the food bolus is transferred from the pharynx above to the stomach below. By virtue of the anti-reflux function, regurgitation of food and liquids is prevented from below upwards.
A third complementary function is secretion. Oesophageal secretions are mucoid in nature to facilitate swallowing. The mucus in the upper part of the oesophagus prevents excoriation of the mucosa by food, and in the lower part protects the oesophageal wall from digestion by gastric reflux into the esophagus.
The anti-reflux function is mainly mediated by the lower oesophageal sphincter, also known as the gastroesophageal or cardiac sphincter. It is the lowest 3-5 cm of the esophagus. This sphincter is tonically contracted between meals to prevent reflux of gastric contents into the esophagus. It relaxes when a bolus of food reaches it during swallowing, but there is a delay of 2-3 seconds at this area before food enters the stomach. So, this area is particularly vulnerable to damage and ulceration by hot, cold or irritant food.
Large doses of gastrin hormone increase the tone of the lower oesophageal sphincter while the vasoactive intestinal polypeptide (VIP) relaxes it. VIP is the neurotransmitter released by neurons of the myenteric plexus at the lower end of the esophagus to relax the lower oesophageal sphincter to allow the passage of food during swallowing.
Types of normal peristaltic contractions in the oesophagus
Primary peristaltic contractions
These contractions sweep the body of the esophagus from above downwards in response to the act of swallowing and start even before the food reaches the esophagus. They start at the upper end of the esophagus as a continuation of the pharyngeal peristalsis. They travel along the whole length of the esophagus in about 9 seconds (3cm/s).
In the upright position, the bolus of the food usually travels along the esophagus faster than the primary peristaltic wave (4cm/s) because of the effect of gravity and reaches the lower end of the esophagus in about 7 seconds.
Secondary peristaltic contractions
They occur in response to distension of the body of the oesophagus by an ingested bolus or a gastro-oesophageal refluxate. They have a clearing function that empties the oesophageal from food and fluid residues as well as from the normal gastric refluxate. During eating and drinking, both types of peristalsis occur and complement each other.
This type of peristalsis does not necessarily involve the whole oesophagus: it spares the part proximal to the site of distension. If the primary peristaltic wave fails to propel the food down in the esophagus, a secondary peristaltic wave starts at the site of the bolus and propagates down. Secondary waves are repeated until the bolus is driven down into the stomach.
Bilateral vagotomy abolishes the primary and secondary waves in the upper half of the oesophageal, but the peristaltic wave in the lower half of the oesophageal can occur as they could be conducted by the local myenteric plexus. So, with bilateral vagotomy, there is difficulty in swallowing until the bolus passes through the upper part of the oesophageal by the effect of gravity. It has to be a small bolus, soft, and well-lubricated.
Deglutition (swallowing)
Deglutition is the transfer of food from the mouth to the stomach, Various groups of muscles, striated and plain, take part in this highly coordinated action, The start of deglutition is voluntary, but it is completed by reflex actions, The deglutition center is in the medulla oblongata.
Speed of swallowing depends on the consistency of food, Fluids reach the stomach very rapidly (in about 6 seconds), since they traverse oesophagus faster than the oesophageal peristaltic waves, This is due to gravity in the erect posture, but they remain above the cardiac sphincter until a peristaltic wave opens this sphincter whereby the fluid enters the stomach, Semisolids take a longer time than fluids and solid materials are slower than semisolids.
Phases of deglutition
Deglutition is divided into 3 phases to facilitate its description but really once the first phase is started the others follow without an interval in between.
The first (voluntary) phase
Food in the mouth is “voluntarily squeezed or rolled posteriorly into the pharynx by the pressure of the tongue upward and backward against the palate.
The second (pharyngeal) phase
It is an involuntary reflex and starts by the passage of food through the pharynx, It is a very rapid phase which takes about 1-2 seconds, The constrictor muscles of the pharynx contract, with receptive relaxation of the upper oesophageal sphincter, The posterior pillars of the fauces approximate to shut off the mouth cavity from the Pharynx and prevent the back passage of food to it.
Stages
- The tongue pushes the food bolus to the back of the mouth.
- Soft palate elevates to prevent food from entering the nasal passages.
- The epiglottis covers the glottis to prevent the food from entering the trachea and the upper oesophageal sphincter relaxes.
- Food descends into the oesophagus.
Important protective reflexes take place to prevent the passage of food into the respiratory openings:
- Elevation of the soft palate to shut off the posterior nares and prevent the passage of food into the nasal cavity.
- Elevation of the larynx and closure of its opening (glottis) by the epiglottis and posterior part of the tongue and approximation of the vocal cords to guard against the passage of food into the airways.
- Inhibition of respiration by a reflex mechanism (reflex apnea), In anaesthesia, the cough and swallowing centers are depressed and protective reflexes do not occur, Secretion or vomitus may accumulate in the pharynx and enter the trachea leading to choking.
The third (oesophageal) phase
In this involuntary phase, food passes along the oesophagus to the stomach by Oesophageal peristaltic contractions, The movements in the upper third of the oesophagus are rapid while those in the lower third are slow, because the muscles of the upper third are striated and supplied by the vagus nerve while in its lower third are plain and depend on the local plexus of Auerbach, The middle third contains both types of muscles, This phase is helped by mucin and gravity in the erect position.
Nervous pathways in deglutition
The reflexes of the involuntary phases are mediated by:
- Afferents: start from receptors that discharge impulses from the upper pharynx along the 5th, 9th, and 10th cranial nerves.
- Centre: is the deglutition center in the medulla oblongata.
- Efferents: are along the 5th cranial nerve to mylohyoid muscles, the 9th,10th, and 11th cranial nerves to the pharyngeal and oesophageal muscles, and the 12th cranial nerve to the tongue muscles.
You can download Science online application on Google Play from this link: Science online Apps on Google play
Pharynx function, anatomy, location, muscles, structure & Esophagus parts
Tongue function, anatomy & structure, Types of lingual papillae & Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication & Otic ganglion