GIT Motility Disorders symptoms, treatment, Bowel motility test and What causes motility disorder
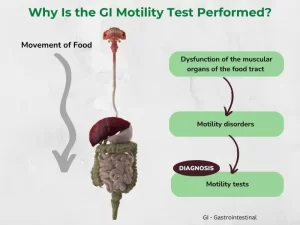
GIT motility disorders refer to conditions where the muscles or nerves in the gastrointestinal (GI) tract don’t function properly. This leads to problems with food and waste moving through the digestive system.
GIT Motility Disorders
The function of the GIT as a digestive o organ depends on three distinct mechanisms working in harmony, namely: secretion, motility, and absorption. It has been estimated that problems or motility may account for about 50% of gastroenterologist’s clinical care load. Many of the underlying mechanisms controlling the motility of the gut are not fully understood. However, recent advances in diagnostic methodology and electrophysiological measurements of the gut’s activities have provided new insights.
Esophageal Motility Disorders
Function of the esophagus
- Transfer function.
- Anti-reflux function.
Types of esophageal peristalsis
- Primary (swallow-induced) peristalsis.
- Secondary (distention-induced) peristalsis.
Pressure measurements of the normal esophagus
UES:
- Resting pressure =100mmHg.
- Pressure during relaxation = Zero or below
Body of the Esophagus
- Resting pressure = – 5 mmHg.
- Pressure during contraction = 30-180mmHg.
LES:
- Resting pressure = 20-40mmHg.
- Pressure during relaxation = SmmHg.
Manometric criteria of Normal Esophageal Contractions
- Sequential or peristaltic form above downwards.
- Amplitude of 30-180mmHg.
- Duration of 2-6 seconds.
- Single and occasionally double-peaked.
Manometric classification of Esophageal Motility Disorders
Abnormalities of esophageal peristalsis:
- Diffuse esophageal spasm (OES).
- Nutcracker esophagus.
- Non-specific esophageal motility disorders (NEMD).
- Aperistaltic esophagus
Abnormalities of LES resting pressure:
- Hypertensive LES.
- Hypotensive LES.
Abnormalities of LES relaxation:
- Incomplete relaxation (achalasia).
- Spontaneous relaxation (GERD).
Abnormalities of UES relaxation:
- Primary achalasia of crico-pharyngeus.
- Secondary relaxation failure due to systemic neurological diseases.
Clinical presentation of Esophageal Motility Disorders
- Asymptomatic cases.
- Cases dominated by pain.
- Cases dominated by dysphagia.
- Complicated cases.
Protocol of Investigations
- Cardiac assessment.
- Radiology (barium swallow and meal).
- Upper endoscopy.
- Esophageal manometry and/or prolonged ambulatory pH monitoring.
Treatment
Defective transport function:
- Reassurance.
- Pharmacological therapy: nitrates calcium-channel blockers.
- Pneumatic dilatation.
- Esophago-cardiomyotomy.
Defective anti-reflux function:
- Reassurance.
- Anti-secretory drugs.
- Prokinetic.
- Anti-reflux surgery.
GI Transit
Regulated smooth muscle contractions result in coordinated changes in gut intraluminal pressure, which controls the transit of the chyme through the GIT.
Each of the major secretions of the GIT has a specific function that requires a different transit pattern. A pressure amplitude gradient, rather than a frequency gradient, determines the transit for each part of the GIT.
Circular contractions
Segment the lumen, mixing the contents continually to expose the mucosa to different contents.
The longitudinal muscles
Shortens the bowel, moving intraluminal contents forward.
The motor migratory complex (MMC)
- Phase 1: is a period of inactivity.
- Phase 2: is a period of intermittent phasic contraction similar to the post-prandial pattern.
- Phase 3: is a continuous period of contractions that are at slow wave frequency, specific for that region of the bowel.
Sphincters are high-pressure zones interposed through the GIT. Contraction or relaxation of the sphincters is controlled by enteric neurotransmitters or by circulating peptide hormones, in response to changes in pressure of the surrounding bowel or physiologic stimuli. Proximal distention relaxes all sphincters, while distal distention contracts sphincters.
Gastric motility disorders
Delayed gastric emptying:
- Post vagotomy.
- Diabetes mellitus.
- Viral infections.
- Reflux esophagitis.
- Brain stem lesions.
- Anorexia nervosa.
Rapid gastric emptying:
- Dumping syndrome.
- Pancreatic insufficiency
- Celiac sprue.
- Zollinger-Ellison syndrome.
- Duodenal ulcer.
- Tachygastria.
Pathogenesis of colonic motility disorders
Slow transit:
Increased segmenting contractions:
- Primary constipation.
- Irritable bowel syndrome (spastic).
- Diverticular disease.
- Anal outlet obstruction.
- Congenital (segmenting – Hirschsprung disease).
Decreased segmenting contractions:
- Irritable bowel syndrome (inertia).
- Primary colonic pseudo-obstruction.
- Diabetes mellitus.
- Progressive systemic sclerosis.
- Spinal cord injury.
Rapid transit:
- Functional diarrhea.
- Bile salt diarrhea.
- Surreptitious abuse of laxatives.
Small intestinal motility disorders
Decreased motility
- Hollow visceral myopathy (primary intestinal pseudo-obstruction).
- Progressive dystrophy.
- Hypothyroidism.
- Jejunal diverticulosis, jejunoileal bypass.
Increased or uncoordinated motility
- Primary visceral neuropathy.
- Carcinoma-associated visceral neuropathy.
- Progressive systemic sclerosis.
- Irritable bowel syndrome.
- Diabetes mellitus.
- Infectious diarrhea.
- Mass lesion of the brain stem.
- Amyloidosis.
- Carcinoid syndrome.
- Hyperthyroidism.
- Shy-Drager syndrome.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach