GIT Bleeding symptoms, causes, types, and How is GI bleeding treated?
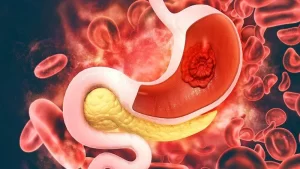
GIT bleeding is a term used to describe bleeding that occurs anywhere within the gastrointestinal (GI) tract, from the mouth to the anus. Upper GI bleeding originates above the ligament of Treitz (part of the small intestine). Lower GI bleeding originates below the ligament of Treitz.
Causes of GIT Bleeding
The cause of GIT bleeding varies depending on its location. Some common causes include:
- Peptic ulcers.
- Inflammatory bowel disease (IBD).
- Diverticular disease.
- Hemorrhoids.
- Colon cancer.
- Esophagitis.
- Gastritis.
Symptoms of GIT Bleeding
They may include:
- Vomiting blood (hematemesis).
- Black, tarry stools (melena).
- Bright red blood in stools (hematochezia).
- Abdominal pain.
- Weakness.
- Dizziness.
- Fatigue.
Diagnosis and Treatment
If you experience symptoms of GIT bleeding, it’s crucial to seek medical attention immediately. Diagnostic tests may include:
Treatment may involve:
- Medications.
- Endoscopic procedures.
- Surgery.
- Blood transfusions.
Types of GI Bleeding
- Upper.
- Lower.
- Occult.
- Obscure.
GI bleeding reclassified into:
- Upper GI bleeding: Mouth to ampulla
- Mid-gut bleeding: Ampulla to the ileo-caecal valve.
- Lower GI bleeding: Colonic bleeding.
1. Upper GI bleeding
Etiology of acute upper GIT bleeding in adults:
Ulcerative or erosive:
1. Peptic ulcer disease.
- Idiopathic.
- Drug-induced (Aspirin, NSAIDs).
- Infectious (H. pylori, Cytomegalovirus, Herpes simplex virus).
- Stress-induced ulcer.
- Zollinger Ellison syndrome.
2. Esophagitis
- Peptic.
- Infectious (Candida albicans, Herpes simplex virus, Cytomegalovirus, Miscellaneous).
- Pill-induced (Alendronate, Tetracycline, Quinidine, Potassium chloride, Aspirin, NSAIDs).
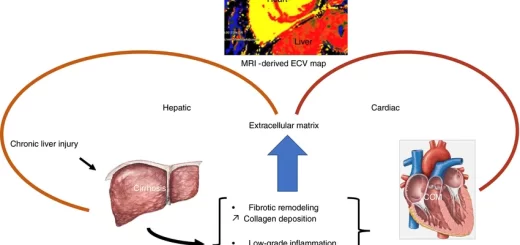
Portal Hypertension
- Esophageal varices.
- Gastric varices.
- Duodenal varices.
- Portal hypertensive gastropathy.
Arterial, venous, or other vascular malformations
- Idiopathic angiomas.
- Hereditary hemorrhagic telangiectasia (Osler-Weber Rendo syndrome).
- Dieulafoy’s lesion.
- Watermelon stomach (gastric antral vascular ectasia).
- Radiation-induced telangiectasia.
- Blue rubber bleb nevus syndrome.
Traumatic or post-surgical
- Mallory-Weiss tear.
- Post-surgical anastomosis.
- Foreign body ingestion.
- Post gastric/duodenal polypectomy,
Tumors
- Benign: Leiomyoma, Lipoma, Polyp, (Hyperplastic, adenomatous, hamartomatous).
- Malignant: Adenocarcinoma, Mesenchymal neoplasm, Lymphoma, Kaposi’s sarcoma, Carcinoid. Melanoma, Metastatic tumor.
- Miscellaneous: Haemobilia, Hemosuccus pancreaticus.
Acute management of severe upper gastrointestinal bleeding
- Resuscitation and stabilization, initiation of medical therapy with an intravenous proton pump inhibitor.
- Assessment of onset and severity of bleeding.
- Risk stratification using a validated prognostic scale.
- Diagnostic endoscopy: Preparation for emergent upper endoscopy localization and identification of the bleeding site identification of stigmata of recent hemorrhage stratification of the risk for rebleeding.
- Therapeutic endoscopy: Control of active bleeding or high-risk lesions Minimization of treatment-related complications, Treatment of persistent or recurrent bleeding.
Role of Endoscopy in Portal Hypertension
- Diagnosis: Presence. Assessment of severity, Prediction of bleeding (Primary Prophylaxis), and PHG.
- Therapeutic: Treatment of bleeding, Prevention of recurrent, Bleeding (secondary prophylaxis), Follow-up, and PHG.
Endoscopic Classification of Esophageal Varices
- The Paquet system attempts to identify patients who are likely to bleed from varices to be candidates for prophylactic EST.
- The package’s classification is four grades.
Diagnostic Endoscopy
- Predictors of Progression of Cirrhosis: Alcoholic, Child B or C, Red Wale signs.
- Variceal Size > 5 mm = Predictor o of bleeding.
Primary Prophylaxis
- B- blocker therapy = Standard.
- Hemodynamic responders = HVPG < 12 or 20% less than original.
- Rebleeding: Responders = 10%. Non-responders = 64%.
- Survival: Responders = 95%. Non-responders = 52%.
- Prophylactic EST = Inappropriate option.
- Prophylactic EVL = A potentially attractive: Equally effective to B-blocker, Indicated in: Sensitive to B-blocker, Contraindication to B-blocker, Hemodynamic “Non-responders.”
Goals and principles of managing Variceal Hemorrhage
Goals of management:
- Prevent first bleed.
- Control acute bleeding.
- Prevent recurrent bleeding.
Principles of management:
- Reduce portal pressure.
- Pharmacologic therapy.
- Surgical or interventional (TIPS) shunts.
- Local control, obliteration of varices.
- Balloon tamponade.
- Endoscopic sclerotherapy.
- Endoscopic ligation (banding).
- Surgical devascularization (Transection. Sugiura procedure).
Rebleeding
- >1.5 g/dl.
- Recurrent hematemesis.
- Rec. or increased frequency,
- Melena or Hematochezia.
Management of Bleeding P.H
- Pharmacologic Therapy: Somatostatin, Octreotide, Terlipressin.
- Balloon Tamponade: (Sungestaken tube).
- Endoscopic.
- TIPS.
- Surgery.
Endoscopic Therapy
Endoscopy Cornerstone management of upper GI Bleeding:
- Diagnostic.
- Therapeutic.
Rates of success & complications:
- Experience of the operator.
- Technique employed.
Therapeutic Endoscopy in P.H:
- Esophageal Varices: Sclerotherapy, Multi-Band Ligation, Tissue Adhesive, Other.
- Gastric Varices (Duodenal, Rectal ): Tissue Adhesives.
- Gastric Varices (GOV1, GOV2, IGV1, IGV2): Tissue Adhesives, Other.
- PHG: APC.
Sclerotherapy in Acute bleeding:
- EST treatment of choice for active variceal hemorrhages,
- EST achieves control in 60% – 100% (90%).
- The major drawback of EST = Complications.
Complications of Sclerotherapy
- Minor: Chest pain, Temporal dysphagia, Fever, Pleural effusions, Strictures.
- Serious (Uncommon): Bacterial peritonitis, Perforation, Mediastinitis, Brain abscess, Spinal cord paralysis, Pericarditis, Portal vein thrombosis, Aspiration pneumonia.
- Complications Related to Technique: Volume of sclerosant at the injection site, Advanced liver disease patients prone to severe ulcers (Control of bleeding is usually difficult, and Severe coagulopathy results in oozing after injections.
Endoscopic Variceal Ligation
Multiple-band devices have now replaced the original single-band device, thereby allowing deployment of 6-10 bands with a single esophageal intubation.
Complications of Variceal Banding (EVL)
- EVL = Same sedation required for EST.
- All Complications are less in EVL than EST: Strictures, Bleeding from treatment-induced ulcers, Pulmonary infection, Bacterial peritonitis, and Death.
- Multiple-band ligatures prevented complications of overtube.
EVL vs EST
- Less complications.
- More effective.
- Better in preventing rebleeding.
- Less number of sessions till eradication
- Not suitable for active bleeding.
- More Recurrence.
- Expectant management alone, the risk of recurrent variceal bleeding is 47% – 84%.
Endpoints of Therapy
- Obliteration of varices.
- The recurrence of varices and bleeding risk were significantly reduced if the varices were either obliterated or persisted as small white columns.
- Persistent small bluish varices were associated with a continued risk of bleeding.
Schedule of Therapy
After control of bleeding, a follow-up session 2-3 days later is a common practice, usually followed by weekly or biweekly procedures until variceal obliteration. Surveillance for the reappearance of varices is usually conducted at intervals that extend from 1-3 months and 6 monthly.
Recurrence of Varices after Variceal Obliteration
- 15-20%.
- Causes not known.
Failure of endotherapy
Definite:
- Inability to control acute bleeding from varices.
- Recurrent bleeding after variceal obliteration.
- Death related to bleeding or Rx complications.
Indefinite:
- Inability to obliterate varices.
- Nonfatal complications of the treatment.
- Recurrent bleeding before obliteration.
Two bleeding episodes while a patient is undergoing Endotherapy by an experienced endoscopist.
Factors Predict Failure of endotherapy
- 10-30%: Gastric fundal varices, Other varices (Colon, duodenum, and unusual locations), and PHG.
- TIPS.
- SURGERY (Shunt).
- TRANSPLANTATION.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Malabsorption syndrome causes, Symptoms, Treatment and How do you fix malabsorption syndrome?
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach