Gastrointestinal tumors symptoms, Esophageal tumors types and treatment
Gastrointestinal (GI) tumors are abnormal growths that develop in the digestive system, This system includes the mouth, esophagus, stomach, small intestine, large intestine (colon), rectum, and anus.
Types of GI Tumors
GI tumors can be divided into two main categories:
- Benign Tumors: These are non-cancerous growths that do not spread to other parts of the body. Examples include polyps, leiomyomas, and adenomas.
- Malignant Tumors (Cancer): These are cancerous growths that can invade nearby tissues and spread to other parts of the body (metastasis). Examples include colorectal cancer, gastric cancer, pancreatic cancer, and esophageal cancer.
Symptoms of GI Tumors
Common symptoms include:
- Abdominal pain or discomfort.
- Changes in bowel habits (diarrhea, constipation, or blood in stool).
- Indigestion or heartburn.
- Nausea and vomiting.
- Weight loss.
- Fatigue.
- Loss of appetite.
It’s important to note that these symptoms can also be caused by other conditions, so it’s crucial to consult a healthcare professional for an accurate diagnosis.
Diagnosis and Treatment
- Diagnosing GI tumors often involves a combination of tests, such as:
- Blood tests.
- Endoscopy (examining the GI tract with a flexible tube)
- Colonoscopy.
- CT scan.
- MRI scan.
- Biopsy (taking a sample of tissue for examination).
Treatment may include:
- Surgery.
- Chemotherapy.
- Radiation therapy.
- Targeted therapy.
- Immunotherapy.
While not all GI tumors can be prevented, maintaining a healthy lifestyle can reduce the risk of developing some types of GI cancer. This includes:
- Eating a balanced diet rich in fruits, vegetables, and whole grains.
- Maintaining a healthy weight.
- Regular exercise.
- Limiting alcohol consumption.
- Not smoking.
Tumor
- Tumor: uncontrolled proliferation of the cells which may be benign or malignant.
- Benign tumor: cells grow as a compact mass and remain at their site of origin.
- Malignant tumor: The growth of cells is uncontrolled, and the cells can invade nearby tissues or organs and spread to distant sites.
Tumors of the GI tract are classified based on their tissue of origin and primary site of development. Both benign and malignant tumors can be found within all these categories.
Risk factors of cancer
They can be roughly divided into environmental factors and genetic factors.
Environmental factors
- It has long been known that the incidence of cancer differs according to the region, occupation, eating habits, and lifestyle.
- Such differences occur due to variations in carcinogens in the environment which induce mutations in some genes.
Examples of environmental risk factors
- Chemical as tobacco.
- Physical as ionizing radiation.
- Biological as viruses.
They lead to mutation in genes controlling cell proliferation.
Genetic factors
- Carcinogenesis is often sporadically observed but sometimes concentrates in certain families. The causes were unknown for many years.
- Studies identified genes responsible for hereditary neoplastic syndrome. DNA repair genes, DNA mismatch repair.
- Hereditary nonpolyposis colon cancer (HNPCC) is a hereditary neoplastic disease that occurs in individuals with abnormalities in DNA mismatch repair genes.
- Normally, adenine and thymine or cytosine and guanine are paired by hydrogen bonds and form DNA double-helices. When a base is substituted by another inappropriate base which forms a mismatch with the other base during DNA replication, the base pair will be removed from the strand and the DNA strands will be repaired.
Esophageal tumors
- Represent about 5 % of all GI tumors.
- The mean age at diagnosis is 60 years.
Types
The two most common malignant types are squamous cell carcinoma and adenocarcinoma.
Squamous cell carcinoma
Incidence and epidemiology
- The most common malignant tumor of the esophagus.
- Male: female = 3:1.
- The commonest site is in the mid and distal esophagus.
Etiology and pathogenesis
Environmental risk factors:
- Tobacco smoking.
- Vitamin deficiencies (A, C, E, B12, folic acid).
- Trace elements deficiencies (selenium, zinc, molybdenum) i.e., poor consumption of green and yellow vegetables.
Other risk factors
- Achalasia of the cardia (a disease characterized by the failure of relaxation of the lower esophageal sphincter ± absence of peristalsis of the body leading to dilation of the esophagus and accumulation of food in it).
- Exposure to ionizing radiation.
- Cancers of head and neck.
- (Tylosis (autosomal dominant – hyperkeratosis of palms and soles).
- Plummer-Vinson Syndrome (a disease affecting middle-aged females characterized by upper esophageal web, iron deficiency anemia, and spooning of nails).
Adenocarcinoma of esophagus
Incidence and epidemiology
- Increasing in the U.S. by 20% every year.
- Higher incidence in U.K. Australia, and Holland.
- White males > 40 years.
- Common in the distal esophagus.
Risk factors
- Obesity (BMI >30 versus <22 = risk 17 folds).
- Gastroesophageal reflux disease complicated with Barrett’s esophagus (the esophageal mucosa with stratified squamous epithelium is replaced with intestinal epithelium with goblet cells due to chronic irritation of esophageal epithelium by acidic reflux of gastric contents).
- Diet (high red meat and fat and deficient minerals and trace elements due to poor consumption of fresh vegetables and fruits).
- Smoking.
- Scleroderma.
Gastroesophageal Reflux→ metaplasia→ low-grade dysplasia → high-grade dysplasia→ adenocarcinoma
Esophageal adenocarcinoma and reflux disease
- Frequent symptoms of reflux are associated with an increased risk of adenocarcinoma.
- The presence of Barrett’s esophagus (intestinal metaplasia with specialized columnar epithelium) is the most important risk factor.
Barrett’s esophagus: length ≥1 cm of a salmon-pink mucosa extending above the esophageal gastric junction accompanied by the presence of intestinal metaplasia (IM) at histology.
Screening is the mechanism through which populations may be assessed to identify individuals who have a disease or a preclinical condition that predisposes them to a disease.
Surveillance is the program through which those at-risk individuals are periodically assessed or examined to identify disease at a stage amenable to cure.
Endoscopic surveillance of Barrett’s esophagus
Who should be screened?
Screening for BE may be considered in men with chronic (>5 years) and/or frequent (weekly or more) symptoms of gastroesophageal reflux disease (heartburn or acid regurgitation) and two or more risk factors for BE or esophageal adenocarcinoma.
These risk factors include:
- Age >50 years, Caucasian race.
- Presence of central obesity (waist circumference >102 cm or waist-hip ratio (WHR) >0.9).
- Current or past history of smoking.
- Confirmed family history of Barrett Esophagus or Esophageal Adenocarcinoma (in a first-degree relative) (strong recommendation, moderate level of evidence).
Management of Barrett’s esophagus
- Patients with BE should receive once-daily proton pump inhibitor therapy.
- If low-grade or high-grade dysplasia is present on EMR, patients should proceed to have endoscopic ablative therapy, with radiofrequency ablation (RFA) being the most cost-effective method.
- Following successful endoscopic treatment and complete elimination of intestinal metaplasia, endoscopic surveillance should be continued to detect recurrent intestinal metaplasia/and or dysplasia.
- Endoscopic surveillance should employ four-quadrant biopsies at 2 cm intervals in patients without dysplasia and 1 cm intervals in patients with prior dysplasia. (Seattle protocol).
- For patients with high-grade dysplasia (or intramucosal carcinoma), repeated endoscopy should be performed every 3 months for the first year, every 6 months for the second year, and annually thereafter.
- In patients with low-grade dysplasia (present before ablation), repeated endoscopy should be performed every 6 months in the first year, and annually thereafter.
Clinical features of cancer esophagus
- Progressive dysphagia (starts for solids then for solids and liquids).
- Odynophagia.
- Weight loss.
- Nausea, vomiting, and hematemesis.
- Involvement of adjacent structures (chronic cough, hoarseness).
- Metastasis (hepatomegaly, bony pains, left supraclavicular adenopathy).
Investigations
Endoscopy: For detection of esophageal tumors and biopsy lesions.
Barium swallow: Persistent filling defect stenosis.
For staging of tumor
Both 2 and 3 are used for distant metastasis
TNM classification for staging (for enrichment)
T categories
- Tx: The primary tumor can’t be assessed.
- TO: There is no evidence of a primary tumor.
- Tis: The cancer is only in the epithelium (the top layer of cells lining the inside of the esophagus). It has not started growing into the deeper layers. This stage is also known as high-grade dysplasia.
- T1a: The cancer is growing into the lamina propria or muscularis mucosa (the tissue under the epithelium).
- T1b: The cancer has grown through the other layers and into the submucosa.
- T2: The cancer is growing into the thick muscle layer (muscularis propria).
- T3: The cancer is growing into the outer layer of the esophagus (the adventitia).
- T4a: The cancer is growing into the pleura (the thin layer of tissue covering the lungs), the pericardium (the thin sac surrounding the heart), or the diaphragm (the muscle below the lungs that separates the chest from the abdomen).
- T4b: The cancer has grown into the trachea (windpipe), the aorta (the large blood vessel coming from the heart), the spine, or other crucial structures.
N categories
- NO: The cancer has not spread to nearby lymph nodes.
- N1: The cancer has spread to 1 or 2 nearby lymph nodes.
- N2: The cancer has spread to 3 to 6 nearby lymph nodes.
- N3: The cancer has spread to 7 or more nearby lymph nodes.
M categories
- MO: The cancer has not spread (metastasized) to distant organs or lymph nodes.
- M1: The cancer has spread to distant lymph nodes and/or other organs. (Common sites of spread include the liver and lungs.)
Treatment
Options include
➤ Endoscopic
- (Endoscopic mucosal resection (EMR) (Endoscopic submucosal dissection) (ESD).
- Stage 1A (T1a NOMO).
- Small lesions that meet the following criteria may be amenable to endoscopic resection (ER): diameter less than or equal to 2 cm, involve less than one-third of the circumference of the esophageal wall and are limited to the mucosa.
➤ Surgical
Stage T1b-stage III.
esophagectomy, preoperative chemoradiation, and definitive chemoradiation.
➤ Palliative
- Stage IV (any T or any N + M1).
- Endoscopic insertion of the stent.
- Systemic chemotherapy with palliative/supportive care.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Malabsorption syndrome causes, Symptoms, Treatment and How do you fix malabsorption syndrome?
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
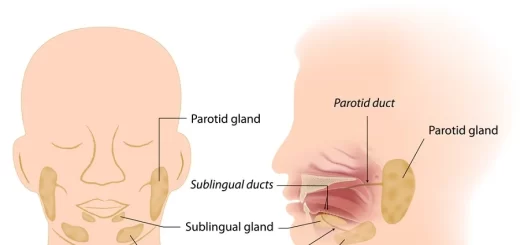
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach