Gastroesophageal reflux disease (GERD) cause, treatment and How to treat eosinophilic esophagitis?
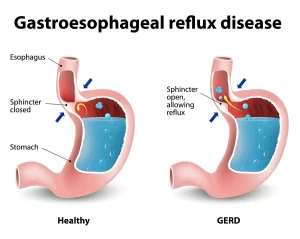
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid flows back up into the esophagus, the tube connecting your mouth and stomach, This backwash is known as acid reflux, and it can irritate the lining of the esophagus.
Gastroesophageal reflux disease
Reflux of gastric contents into the esophagus (is a condition where gastric acid comes up from the stomach into the esophagus).
Etiology
GERD results from the incompetence of the lower esophageal sphincter.
Factors which contribute to the competence of GE junction (High-Pressure Zone) include:
- Intrinsic sphincter pressure.
- The angle of cardio-esophageal junction
- The action of the diaphragm.
- Gravity.
- Local neutralizing effect of saliva.
GERD leads to esophagitis (damage to the esophageal mucosa) due to:
- Caustic nature of the refluxate and the inability to clear the refluxate from the esophagus.
- Volume of gastric contents.
- Decrease local mucosal protective mechanism.
The condition is predisposed by:
- Obesity.
- Excessive intake of a fatty diet, chocolate, coffee, and cola drinks.
- Smoking and drugs (anticholinergic drugs NSAIDs).
- Diseases such as systemic sclerosis, achalasia, and hiatal hernia.
Clinical picture
- Heart Burn (Pyrosis): Feeling of substernal burning pain that radiates upward from the epigastrium toward the neck occurring within one hour after meals and increased by a maneuver that increases the intra-abdominal pressure.
- Odynophagiar (Substernal pain on swallowing) may occur in esophagitis (long-standing reflux).
- Stricture and dysphagia.
Diagnosis
- Barium swallow: shows reflux, stricture, ulcer, achalasia, and hiatal hernia.
- Upper endoscopy: Identifies the degree of GERD (LA Classification) to rule out stricture, ulcer, achalasia, hiatal hernia, and to take a biopsy from GE junction to rule out the presence of Barret’s esophagus.
- Esophageal manometric study: May show decreased tone of the LES.
- Bernstein acid perfusion test: Simulation of GER by instillation of 0.1 N HCI into the lower esophagus.
Complications
- Peptic stricture which can lead to dysphagia.
- Hematemesis from peptic ulceration of the lower esophagus.
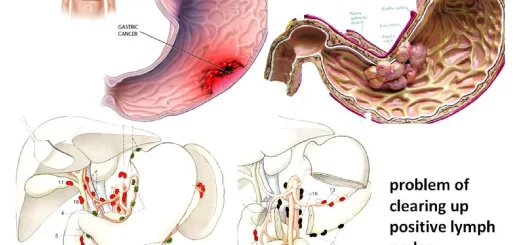
- Barrett’s esophagus: Barrett’s esophagus is a serious complication of GERD which is a premalignant condition. It is a simple columnar metaplasia in the cells of the lower portion of the esophagus. It is characterized by the replacement of the normal stratified squamous epithelium lining of the esophagus by simple columnar epithelium with goblet cells (which are usually found in the lower gastrointestinal tract). The medical significance of Barrett’s esophagus is its strong association (about 0.5% of patients/year) with esophageal adenocarcinoma.
Treatment
- Lifestyle modifications: Decrease body weight, Avoid fatty diet, and acidic foods, Avoid sleeping after meals, Elevation of the head of the bed by 6 inches, Stop smoking, drugs, chocolate, coffee, and cola as they decrease L.E.S pressure.
- H2 Blockers: (Cimitidine, Ranitidine, Fomotidine, Nizatidine).
- Proton Pump inhibitors: (Omeprozol, Pantoprozol, Lanzoprozol, Esomeprazole, Dexalanzo-Rabepraz) to decrease gastric acidity.
- Prokinetic drugs to strengthen LES: Cholinergic agonists (Bethanecol 25 mg 3 times), Metoclopropamide 10 mg 3 times, Domperidone, Itopride.
- Treatment of Helicobacter Pylori infection.
- Treatment of complications:
- Hemorrhage unless massive does not require emergency surgery.
- Esophageal stricture: dilatation with Hg-filled Bougies or with endoscopically placed balloons.
- Resistant cases: Surgery as fundoplication which can be performed laparoscopically.
- Barret’s esophagus: Intensive medical therapy or surgically, with follow-up endoscopically.
Hiatal Hernia (HH)
Protrusion of the stomach above the diaphragm.
Types of HH
- Sliding HH.
- Paraesophageal HH.
Sliding HH
- The gastroesophageal junction slides through the hiatus so that lies above the diaphragm.
- Common seen by x-ray in 40% of the population.
- Most patients are asymptomatic.
- Might produce chest pain.
- GERD occurs in few patients
- Occult or massive GIT hemorrhage may occur with either type of HH.
Paraesophageal HH
- A small part of the stomach rolls up through the hiatus alongside the esophagus. The GE junction remains below the diaphragm.
- Asymptomatic but may incarcerate or strangulate.
Diagnosis
Barium study/endoscopy
Treatment
- Antacids – H2 Blocker.
- Surgery for paraoesophageal HH for fear of the risk of strangulation.
Mallory Weiss Syndrome
- Linear mucosal tear occurring at the esophagogastric junction and produced by a sudden increase of the intra-abdominal pressure after bouts of cough or vomiting producing hematemesis which usually stops spontaneously. Rarely, blood transfusion & injection of adrenaline endoscopically is required.
- May occur in alcoholics and bulimics (bulimia nervosa patients = fear of obesity).
Boerhaave’s syndrome (Esophageal perforation)
- After forcible instrumentation (endoscope), causing severe epigastric pain and lower substernal pain radiating to the back with minimal hematemesis and surgical emphysema.
- Fatal conditions need thoracotomy and closure of the perforation.
Eosinophilic esophagitis (EoE)
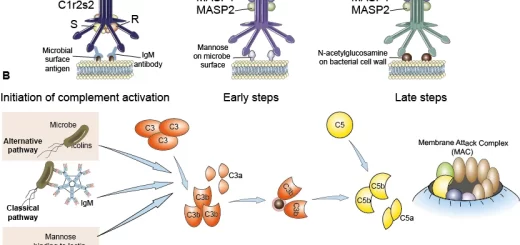
EoE represents a chronic, immune/antigen-mediated, esophageal disease characterized clinically by symptoms related to esophageal dysfunction and histologically by eosinophil-predominant inflammation.
Prevalence:
- Atopic male (male/female ratio 2:1 to 3:1) presents in childhood or during the third or fourth decades of life.
- White, non-Hispanic.
- Prevalence is increasing at a rate of 6-30 cases/100,000.
- EoE in the United States 52/100,000.
Diagnostic criteria (Gastroenterology Consensus 2007):
- Esophageal symptoms
- >15 Eosinophils per HPF (X400).
- Lack of response to PPI.
- Normal pH monitoring.
Presentation of EoE
- Dysphagia is the most common symptom (15% of patients with dysphagia have EOE on random biopsies.
- Food impaction is even more common.
- Refractory GERD is an important presentation (1- 4%).
Endoscopic findings
- Fixed esophageal rings (corrugated rings or (trachealization).
- Transient esophageal rings (feline folds or felinization).
- Whitish exudates and mucosal edema.
- Longitudinal furrows.
- Diffuse esophageal narrowing.
- Narrow-caliber esophagus.
- Esophageal lacerations by the passage of the endoscope.
Bullous esophagitis
Bullous esophagitis is an uncommon cause of esophagitis. Nevertheless, awareness of this condition is important to make a diagnosis and institute appropriate therapy.
Many autoimmune skin disorders also affect the esophagus, as both skin and esophagus are covered with squamous epithelium.
Patients with bullous esophagitis may present with a spectrum of symptoms including odynophagia, dysphagia, hematemesis, and vomiting of esophageal casts of squamous epithelia.
Owing to the fibrosing nature of these disorders, patients can develop strictures of the esophagus. The diagnosis of bullous esophagitis is established by a combination of clinical examination, laboratory data, endoscopy, and histology.
On EGD, patients with bullous esophagitis often have a normal-appearing esophageal mucosa, but on touching this with the endoscope, bulla forms rapidly. This may be called the endoscopic Nikolsky sign. Therapy for bullous esophagitis is directed at the specific underlying cause. For autoimmune sub-epidermal blistering diseases, the therapy of choice is systemic steroids.
Esophagitis dissecans superficialis (Sloughing esophagitis)
Esophagitis dissecans superficialis (EDS) is a term applied to a rare endoscopic finding characterized by sloughing of large fragments of the esophageal squamous mucosa that may be coughed up or vomited.
EDS affects older people debilitated patients on multiple medications, people with malignant disease on chemotherapy and after chemical injuries (toxic dose of drugs) and physical injuries (burns), electric shocks, bedridden, hospitalized, or malnourished patients, patients having metastatic cancer, organ transplantation, and/or being immunosuppressed.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach