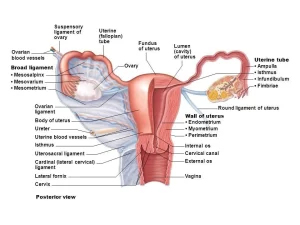
Female reproductive system organs, functions, anatomy and Histological structure of the uterus
The female reproductive system consists of primary sex organs, which are the two ovaries, and secondary sex organs, which include: The female reproductive tract is composed of (two Fallopian tubes (oviducts or uterine tubes), uterus, cervix, and the vagina), The external genitalia, and the accessory sex organs, which are (placenta, and mammary glands).
Female external genital organs
The female external genitalia are collectively referred to as the vulva, they include:
- Mons pubis: an anterior thick skin fold, having a collection of subcutaneous fat, hairy.
- Labia majora: two rounded thick skin folds, one on each side. The space between these folds is called the pudendal cleft. These skin folds have a hairy outer surface and Inner surface devoid of hair. They enclose an abundant amount of adipose tissue and a thin layer of smooth muscle fibers. The skin of labia majora is richly supplied by sensory nerve endings and contains numerous sebaceous and sweat glands.
- Labia minora: Two thin skin folds, one on each side, The space between these folds is called the vestibule of the vagina, They lack hair follicles but they have numerous sebaceous glands, They enclose a core of loose connective tissue rich in elastic fibers and sensory nerve endings.
- Clitoris: is an erectile structure covered by stratified squamous epithelium and supported by a lamina propria rich in blood vessels and sensory nerve endings. It resembles the penis in male. It is in the anterior part of the pudendal cleft. It consists of 2 corpora cavernosa (forming the body of the clitoris) which enlarge anteriorly to form the glans clitoris.
- Urethral orifice: it lies between the glans clitoris anteriorly and the vaginal orifice posteriorly.
- Vaginal orifice. it lies posterior to the urethral orifice.
Female internal genital organs
The principal organs of the human female reproductive tract consist of the ovaries, the fallopian tubes, the uterus and the vagina.
Uterus
Definition: It is a pear-shaped hollow muscular organ, that lies between the rectum and urinary bladder inside the pelvic cavity.
Dimensions: its size is 1,2,3 inches (thickness, width, and length respectively).
Parts of the uterus
- Fundus: the upper rounded free part above the level of the openings of the uterine tubes.
- Body: it has 2 surfaces anterior and posterior. It constricts lower down at a constriction called the isthmus to become the cervix.
- Cornua: it is the junction between the fundus and the body. It lies in the lateral angle of the uterus.
- Cervix: It is the lower narrow part that protrudes into the upper vaginal end. It is 1-inch width and length. Its canal is connected to the uterine cavity by an opening called the internal os. Its canal is connected to the vagina by external os.
Position of the uterus
The normal position is anteflexion & anteversion (AVF position). Anteflexed (the forward angle between the long axis of the body of the uterus and that of the cervix = an obtuse angle, 170 degrees). Anteverted (the forward angle between long axis of the vagina and that of the cervix= 90 degrees). If the uterus is directed backwards, it is called retroverted, retroflexed (RVF).
Body of uterus and its relations
It has 2 surfaces. Anterior (vesical) surface is separated from the urinary bladder by the uterovesical pouch. Posterior (intestinal) surface is separated from the rectum by the recto-uterine pouch. (Douglas pouch) coils of the sigmoid colon and terminal ileum are present in this pouch.
Laterally: The lateral border gives attachment to the broad ligament. Uterine artery runs along this border. At the cornua, the uterine tube joins the uterus. Below and in front of the lateral angle of the uterus, round ligament of the uterus is attached. Below and behind the lateral angle of the uterus, the ligament of the ovary is attached.
Cervix
It is the lower part of the uterus and projects into the vagina through the upper part of its anterior wall of the vagina and divides it into:
a. Supravaginal part:
- Anteriorly: has no peritoneal covering, related to the base of the urinary bladder.
- Posteriorly: covered by peritoneum which reflects on the rectum as Douglas pouch.
- Laterally: it gives attachment to broad ligament and is related to Ureter and uterine vessels.
b. Vaginal part:
- Projects through the anterior wall of the agina.
- Surrounded by 4 vagina fornices.
- opens into the vagina by external os.
External os in nulliparous is small and rounded but it is in the form of a transverse slit in the female who has borne babies, and has anterior and posterior lips.
Peritoneal covering of the uterus
The peritoneum is reflected from the lower part of the anterior abdominal wall to cover the upper surface of the urinary bladder, then reflected in front of the uterus at the isthmus, to form uterovesical pouch, then covers the anterior surface of the body of the uterus, fundus of the uterus, posterior surface of body and cervix of the uterus and upper 1/4 of posterior wall of the vagina.
The peritoneum reflects in front of middle 1/3 of the rectum to form a recto-uterine pouch (Douglas pouch). Laterally the peritoneum forms folds that extend from the uterus to the side walls of the pelvis. These folds are known as broad ligaments and contain the uterine tubes in their upper free borders.
Ligaments of the uterus
the first 3 are attached to the cervix:
- Uterosacral ligament: extends from the cervix, and passes around the sides of the rectum to the front of the sacrum.
- Pubocervical ligament: from the junction of cervix and vagina, passes around the urethra to the back of the pubic body.
- Transverse cervical ligament (Cardinal, Mackenrodt’s or lateral cervical): extends from the cervix and lateral fornix of the vagina to the lateral wall of the pelvis.
- Ligament of the ovary: extends from the uterine end of the ovary to the cornua of uterus.
- Round ligament of the uterus: extends from cornua of the uterus, runs within the broad ligament, then enters the inguinal canal to insert into the labia majora.
- Broad ligament: a double-layered fold of peritoneum, extended from the lateral margin of the uterus to the side wall of the pelvis, It has a free superior border, containing the uterine tube, An attached lower border (root), attached to the floor of the pelvis, The ovary is attached to it by a short peritoneal fold called mesovarium.
Parts of the broad ligament
- Mesometrium: between pelvic floor, ligament of the ovary, and body of the uterus.
- Mesosalpinx: between uterine tube and ligament of ovary.
- The suspensory ligament of the ovary is the part that connects the infundibulum of the uterine tube& upper end of the ovary to the pelvic wall, it transmits the ovarian vessels and nerves.
Contents of the broad ligament
- The uterine tube is enclosed in the anterior free border of the broad ligament (all except its fimbriated end).
- Ligaments: Ovarian ligament (posterior surface), and Round ligament of the uterus (anterior surface).
- Arteries: The ovarian artery passes through the suspensory ligament of the ovary to the mesosalpinx then it enters the mesovarium to reach the ovary, and the Uterine artery.
- Embryological remnants: About 15 – 20 rudimentary tubules (epoophoron, paroophoron, and vesicular appendix) are present in the lateral part of the broad ligament between the ovary and the fallopian tube. Gartner’s duct.
- Parametrium, which is a condensation of fatty tissue, autonomic nerves, and lymphatics.
Factors keeping the uterus in position (uterine support)
- Levator ani.
- Ligaments of the uterus.
- Perineal body.
- Urogenital diaphragm.
Weakness of the uterine supports leads to downward descend (telescoping) of the uterus through the vagina (uterine prolapse).
Arterial supply of the uterus
Uterine artery: arises from the anterior division of the internal iliac artery. It has a tortuous course. It runs medially on the floor of the pelvis, in the root of the broad ligament. 2 cm lateral to the cervix; it crosses over the ureter to ascend along the side of the uterus.
Below the uterine tube, it turns laterally to anastomose with the ovarian artery. It supplies the uterus, medial part of the uterine tube, upper vagina, and ureter. It gives vaginal, cervical ureteric, tubal, and anastomotic branches. The uterine artery gives the following branches:
- Vaginal branches.
- Ureteric branches. (to the ureter).
- Cervical branches.
- Uterine branches.
- Tubal branches.
- The anastomotic branch which anastomoses with the branches of the ovarian artery.
Venous drainage: Uterine venous plexus which drains into the internal iliac vein.
Lymph drainage:
- Fundus, upper part of the body → para-aortic LNs (along the ovarian vessels).
- Cornuae → superficial inguinal LNs (along the round ligament).
- Lower part of the body → external iliac lymph nodes.
- Cervix → internal iliac, external iliac, and sacral lymph nodes.
Histological structure of the uterus
The uterine wall is formed of three layers, the endometrium, the myometrium and the perimetrium corresponding to the mucosa, the musculosa and the serosa.
Endometrium
- The surface epithelium: it consists of columnar epithelium that has both ciliated and secretory cells.
- The lamina propria: it consists of highly cellular stroma which contains abundant ground substance. Simple tubular uterine glands which sometimes branch in their deeper portions. The lining cells of the glands are columnar in shape with oval basal nuclei and are secretory in function.
The endometrium is functionally divided into:
- Superficial functional layer: This layer is shed at menstruation and renewed monthly during each menstrual cycle. It is supplied by spiral (coiled) arteries.
- Basal resting layer: This layer is not shed with the menstrual cycle and serves in the regeneration of the functional layer. This layer is supplied by straight arteries.
Myometrium
It is the thickest layer of the uterine wall, composed of bundles of smooth muscle fibers separated by connective tissue. Four interwoven layers can be distinguished:
- The submucosal layer (stratum submucosum): a thin layer formed of longitudinal smooth-muscle fibers.
- The vascular layer (stratum vasculare): the thickest layer of the myometrium formed of oblique muscle fibers arranged around the numerous blood vessels in 8 shaped figures.
- The supravascular layer (stratum supravasculare): thin layer, formed of circularly arranged smooth muscle fibers.
- The subserosal layer (stratum subserosum): thin layer, formed of longitudinal smooth-muscle fibers.
Perimetrium
It is the outer layer of the uterine wall. It is formed of connective tissue covered at certain areas by mesothelial cells according to the uterine anatomical position.
Histological structure of the uterine cervix
The cervix is the lower cylindrical part of the uterus. Its histological structure is differentiated from the rest of the uterus by the following:
The upper part of the cervical canal is lined by endocervical mucosa, formed of:
- Simple partially-ciliated columnar epithelium, similar to the lining of the body of the uterus.
- Thick lamina propria contains mucous cervical glands which are extensively branching.
1. The lower part, which bulges into the vagina, is lined by exocervical mucosa, formed of non-keratinized stratified squamous epithelium, continuous with that of the vagina.
2. The cervical mucosa undergoes little change in thickness during the menstrual cycle and is not sloughed during the period of menstruation.
3. The amount and properties of the mucus secreted by the cervical glands vary during the menstrual cycle under the influence of the ovarian hormones:
- At ovulation, the amount of mucus produced increases and becomes less viscous to provide a more favorable environment for sperm migration.
- In the luteal phase and during pregnancy, the cervical mucus becomes highly viscous (mucous plug) to restrict the passage of sperm into the uterus.
4. The bulk of the cervix is made up of dense, fibrous connective tissue with relatively little smooth muscle.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Fallopian tubes function, location, anatomy & Histological structure of the vagina
Ovary function, location, anatomy, structure, Oogenesis and maturation of primary oocyte
Monthly ovarian cycle, Corpus luteum & menstrual cycle phases, function & hormones
Ovarian hormones, Menopause, Functions of estrogen & progesterone in pregnancy
Female mammary glands (breast), signs of breast cancer & Mammary gland abnormalities