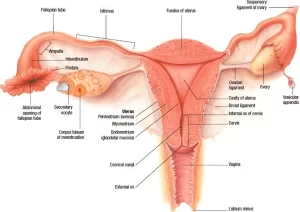
Fallopian tubes function, location, anatomy and Histological structure of vagina
The Fallopian tubes (the oviducts, uterine tubes), each is a 12 cm long musculo-membranous tube showing great mobility. One of its ends opens into the peritoneal cavity next to the ovary; the other crosses the wall of the uterus to open into its interior.
Fallopian tubes
The uterine tube is divided into 4 segments:
- The interstitial part (intramural part): passes through the wall of the uterus.
- The isthmus is adjacent to the uterus.
- The ampulla is longer and more dilated than the isthmus, This is the part where the fertilization of the ovum takes place.
- The infundibulum: It is funnel-shaped and situated near the ovary. It has finger-like extensions (fimbriae) at its free end. Its opening into the peritoneal cavity is called the abdominal ostium. Ovarian fimbria is a large fimbria attached to the ovary. During ovulation, fimbriae trap the non-fertilized ovum and sweep it into the ampulla through the abdominal ostium.
Histological structure of the uterine (Fallopian) tube
The wall of the uterine tube is formed of three layers: the inner mucosa, the middle musculosa, and the outermost serosa. Mucosa has long primary, secondary, and tertiary folds, especially at the region of the ampulla which, in cross-section resembles a labyrinth. It is formed of:
1. The surface epithelium: simple columnar, partially ciliated epithelium, It is composed of two types of cells:
- Ciliated columnar cells, the cilia beat towards the uterus, causing movement of a mucus film that covers the epithelial surface. Movement of the surface mucus film helps the transport of the fertilized ovum towards the uterus, promoted by the muscular activity of the tube. It also prevents the passage of microorganisms from the uterus to the peritoneal cavity.
- Non-ciliated secretory cells interspersed between the ciliated cells and secrete glycoprotein mucous secretion. The glycoprotein secretion covering the mucosa has a protective and nutritive function for both the oocyte and the sperms, including the capacitation factors activating the sperms on their way to reach the ovum for fertilization.
2. The lamina propria: formed of loose vascular connective tissue.
Musculosa: it is moderately thick: and formed of two layers of smooth muscle fibers, inner circular and outer longitudinal. It has a bidirectional transport role: Distending the oviduct towards the ovary to aid in “capturing the ovum by the fimbriae. Producing peristaltic waves which help to propel the ovum towards the uterus.
Serosa: this layer is formed of connective tissue containing large-sized blood vessels (the ovarian and uterine blood vessels) and is covered externally by squamous mesothelial cells (the visceral peritoneum).
There are striking regional variations in the oviduct that reflect the function of each part. In the infundibulum, the lumen is large and filled with many mucosal folds. Progressing towards the uterus, the overall luminal diameter decreases as does the number of ciliated cells, while the smooth muscle fibers of the musculosa gradually increase.
The vagina
The vagina is a fibro-muscular tube that joins the reproductive tract with the external environment. It is from 7cm to 10 cm in length. It descends antero-inferiorly from the cervix of the uterus to the vestibule of the vagina (cleft between the 2 labia minora).
Shape: A tube with 2 walls. The anterior one is shorter (3 inches) while the posterior wall is 4 inches.
Relations: Three structures to each surface:
Anteriorly it is intimately related to the cervix of the uterus, urethra and urinary bladder.
Posteriorly: upper ¼th is covered by the peritoneum of the Douglas pouch, its middle 2/4th are related to the rectum, and its lower ¼th is separated from the anal canal by the perineal body.
Laterally: is related to
- Upper third: lateral fornix is closely related to the ureter, where the ureter is crossed by the uterine artery.
- Middle third: levator ani (pubovaginalis part) and pelvic fascia.
- Lower third: traverse the deep perineal pouch and related to the greater vestibular gland.
Superiorly communicates with the cervical canal. Inferiorly opens into the vaginal vestibule, The walls of the vagina are normally in contact with each other, The posterior wall is longer than the anterior wall, and the posterior wall is in contact with the external os, The vaginal recess around the cervix is called the fornix, There are 4 vaginal fornices:
Two lateral fornices, one on each side, is closely related to: the ureter and uterine artery.
The anterior fornix: is shallow.
The posterior fornix is the deepest one, known as the seminal pool, It is covered by the peritoneum.
Paracentesis: in peritonitis, accumulation of body fluid, blood or, pus in the Douglas pouch of the peritoneal cavity is easily drained through the posterior. fornix of the evagina.
The vaginal vault is separated from the recto-uterine pouch only by a few mm of tissue; care must be taken to avoid penetrating the wall of the rectum by the needle during paracentesis.
Histological structure of vagina
The wall of the vagina consists of three layers:
Mucosa
- The surface epithelium: It is lined by non-keratinized stratified squamous epithelium. Under the effect of estrogen, the vaginal epithelium accumulates a large amount of glycogen which is responsible for the characteristic vacuolated appearance of the vaginal epithelium in H&E histological sections.
- The lamina propria: Formed of loose connective tissue rich in blood capillaries, and elastic fibers, lymphocytes and neutrophils, No glands are present in the vaginal mucosa, The lubricating mucus found in the vaginal lumen comes from the glands of the uterine cervix.
Musculosa
It consists of interlacing bundles of smooth muscle fibers arranged in longitudinal and circular directions.
Adventitia
It is a layer of dense connective tissue, rich in elastic fibers, and contains an extensive venous plexus, lymphatics, and nerve fibers.
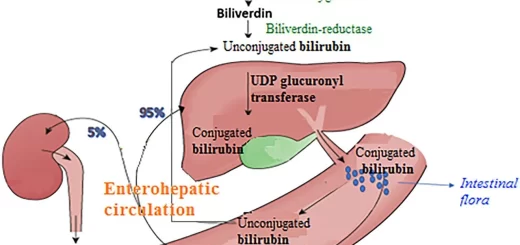
Naturally-occurring vaginal bacterial flora metabolizes glycogen of the desquamated epithelial cells and forms lactic acid, responsible for the normal acidic pH of the vagina. This low pH provides protection against pathogenic microorganisms.
You can download Science online application on google play from this link: Science online Apps on Google Play
Female reproductive system organs, functions, anatomy & Histological structure of the uterus
Ovary function, location, anatomy, structure, Oogenesis and maturation of primary oocyte
Monthly ovarian cycle, Corpus luteum & menstrual cycle phases, function & hormones
Ovarian hormones, Menopause, Functions of estrogen & progesterone in pregnancy
Female mammary glands (breast), signs of breast cancer & Mammary gland abnormalities