Esophagus diseases, Dysphagia causes, Achalasia and Symptomatic Diffuse Esophageal spasm
The esophagus is a key part of the digestive system, It is a muscular tube that carries food from the mouth to the stomach, Several diseases can affect this vital organ, leading to discomfort, difficulty swallowing, and other complications.
Esophagus
- It is a muscular tube approximately (10 inches) 25cm long connecting the hypopharynx to the stomach.
- Lies posterior to the trachea.
- Divided into three parts: Cervical, Thoracic, and Abdominal.
- The muscle coat has 2 layers: an outer longitudinal and an inner circular layer.
- In the upper 1/3, both layers are striated muscle.
- In the lower 2/3, both layers are smooth muscle.
- It is lined by stratified squamous epithelium except below the gastro-esophageal junction where it is lined with columnar epithelium.
- The esophagus is separated from the pharynx by the upper esophageal sphincter (UES) which is usually closed by the continuous contraction of the cricopharyngeus muscle.
- The lower esophageal sphincter (LES) consists of an area of the distal end of the esophagus which has a high-pressure resting zone (~20mmHg) above the gastric baseline and is largely responsible for 2 the prevention of reflux.
Physiology of swallowing
- During swallowing the bolus of food is moved from the mouth to the pharynx voluntarily. Immediately the UES relaxes, and food enters the Esophagus.
- A 1ry peristaltic wave starts at the pharynx to push the food to the LES which relaxes to the gastric baseline allowing the food to pass to the stomach.
- 2ry peristalsis occurs locally in response to distension and helps to clear food residue from the esophagus. Contraction of swallowing in the upper third is central while in the lower, two third is by the local nerve plexus.
Common Esophageal Diseases
- Gastroesophageal Reflux Disease (GERD): This is the most common esophageal disorder, characterized by the backflow of stomach acid into the esophagus. Symptoms of GERD such as heartburn, acid reflux, and difficulty swallowing.
- Achalasia: This is a rare condition where the muscles at the lower end of the esophagus fail to relax, making it difficult to swallow food and liquids.
- Barrett’s Esophagus is a precancerous condition where the lining of the esophagus changes due to chronic acid exposure.
- Esophageal Cancer: This is a serious condition that can occur in the squamous cells or glandular cells of the esophagus.
- Eosinophilic Esophagitis: This is an allergic condition where eosinophils (a type of white blood cell) build up in the esophagus, causing inflammation and difficulty swallowing.
Other Esophageal Disorders
- Esophageal Diverticula: These are pouches that form in the esophagus.
- Esophageal Spasm: This is when the esophagus contracts involuntarily.
- Esophageal Stricture is a narrowing of the esophagus.
- Esophageal Varices: These are swollen blood vessels in the esophagus.
Symptoms of Esophageal Diseases
Symptoms can vary depending on the specific condition but may include:
- Heartburn.
- Chest pain.
- Difficulty swallowing (dysphagia).
- Regurgitation.
- Nausea.
- Vomiting.
- Weight loss.
Diagnosis and Treatment
Diagnosing esophageal diseases often involves a combination of medical history, physical examination, and tests such as endoscopy, barium swallow, and esophageal manometry. Treatment options vary depending on the specific condition and can include:
- Lifestyle changes (diet, weight loss, elevation of the head of the bed).
- Medications (antacids, proton pump inhibitors, etc.).
- Endoscopic procedures.
- Surgery.
Dysphagia
Subjective awareness of difficulty in swallowing due to impaired progression of food from the pharynx to the stomach (difficulty in swallowing) while odynophagia is painful swallowing.
Causes:
- Esophageal motility/structural disorders.
- Extrinsic pressure.
- Intrinsic lesions.
Pre-esophageal (oropharyngeal) causes
- Difficulty in emptying food material from the oropharynx into the esophagus (difficulty in (initiating swallowing).
- lt results from neuromuscular disorders such as: Myasthenia Gravis, Bulbar poliomyelitis, and Pseudobulbar syndrome.
- It is usually associated with nasal regurge, choking, and aspiration pneumonitis.
- On examination: drooling, dysarthria, hoarseness, and neurological deficit are seen.
Esophageal causes
- Motility disorder: Achalasia, Diffuse Esophageal spasm.
- Structural: Benign/malignant stricture, foreign body, rings, diverticulae.
Structural:
- Foreign bodies: Coins, pins, needles, etc.
- Stricture: Benign, GERD, corrosives, radiotherapy, injection sclerotherapy, post band, post-APC, traumatic N.G intubation, and Malignant (carcinoma).
- Lower Esophageal (Ring Shatzki): Narrowing of the lower end of the Esophagus due to a ridge of mucosa or fibrous membrane.
- Upper Esophageal web (Plummer Vinson/Paterson Kelly): Atrophy of the squamous epithelium in the post-cricoid region near the upper sphincter with the formation of the web.
- Dysphagia/Odynophagia
- Iron deficiency anemia.
- Atrophic glossitis.
- Angular stomatitis: It is one of the risk factors for developing squamous cell carcinoma of the oral cavity, esophagus, and hypopharynx.
- Diverticula: Pouch lined in epithelium which can produce dysphagia and regurgitation ( Zenker’s: Upper esophageal (above UES), Traction: mid-esophageal, Epiphrenic: lower esophageal (above LES).
Motor disorders of the Esophagus
Achalasia
- The disease of unknown etiology is characterized by aperistalsis of the body of the Esophagus and failure of relaxation of LES on initiation of swallowing.
- Pathology: Degenerative lesions are found in the vagus nerve supply of the esophagus as well as a decrease of ganglionic cells in the nerve plexus of the esophageal wall.
Clinical picture:
- Occurs at any age usually middle age between 20-40 years.
- Rare disease 1/100,000.
- Gradual onset of dysphagia over months or years.
- Dysphagia for both solids and liquids.
- Other symptoms: regurgitation, chest pain nocturnal cough.
- Predisposes to squamous cell carcinoma.
- Regurgitation of undigested food occurs in 33% and may cause cough, pulmonary aspiration with lung abscess, pneumonia, or bronchiectasis.
- Chest pain on swallowing.
- Weight loss is usually mild to moderate but severe weight loss should suspect pseudo-achalasia 2ry to a tumor of GE junction.
Diagnosis
- Barium swallow: pre-stenotic dilatation of the esophagus with tapering smooth lower end (parrot beak deformity) due to failure of the sphincter to relax.
- Upper endoscopy: Essential to exclude carcinoma of the esophagus. The dilated Esophagus and the endoscope can pass the narrow sphincter to the stomach easily by its weight (with a certain degree of resistance).
- Esophageal manometry: Peristalsis of the body of the Esophagus. Increased pressure of LES.
Treatment
- Long-term nitrates and calcium channel blockers to lower the resting LES pressure.
- Dilatation of LES by pneumatic balloon to weaken LES (Boston regiflex).
- Direct injection of Botulinum toxin into LES (chemical denervation of cholinergic nerves in the distal esophagus).
- Heller’s operation: surgical division of the muscle coat of the lower esophagus sphincter.
- POEM: Per Oesophageal Endoscopic Myotomy.
Symptomatic Diffuse Esophageal spasm
A generalized neurogenic disorder of the esophageal motility in which phasic, non-propulsive contraction replaces normal peristalsis; and in some cases, LES malfunction occurs. This type of spasm is an irregular, uncoordinated squeezing of the muscles of the esophagus.
Clinical Picture
Severe retrosternal chest pain with dysphagia for both liquids and solids. The pain may awaken the patient from sleep. Very hot and cold liquids may aggravate the pain. The disorder may evolve into achalasia.
Diagnosis
- Barium study: May show poor progression of Barium bolus or cork-screw appearance.
- Manometric study: Shows repetitive, high amplitude, non-peristaltic control, or spasm. In 30% of the patients, there is LES pressure and relaxation impairment.
Treatment
- Anticholinergic, Nitroglycin, long-acting nitrates.
- Calcium channel blocker (Verapamil 80 mg 3hrs). Pneumatic dilatation and Bougienage may be helpful.
- Surgical myotomy along the full length of the esophagus in intractable cases.
Extra-esophageal causes
Mediastinal glands, Retrosternal goiter, Enlarged left atrium.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
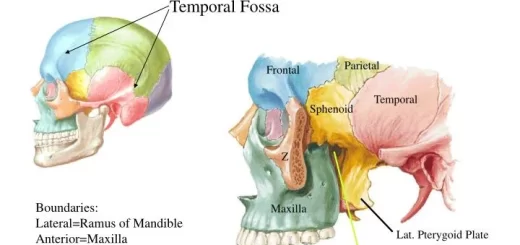
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion