Diagnosis of the cause of jaundice, Hepatobiliary imaging, treatment of cholestasis and Pruritus
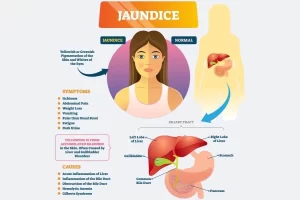
Jaundice is known as hyperbilirubinemia, It is defined as a yellow discoloration of the body tissue resulting from the accumulation of excess bilirubin, Bilirubin deposition takes place only when there is an excess of bilirubin, and this indicates increased production or impaired excretion.
Diagnosis of the cause of jaundice
History
- The age and sex.
- The duration of jaundice, episodic or intermittent, and the presence of contemporary events should be ascertained, such as pain, intercurrent illness, and all medication used (both current and over the past 6 months.
- Recent or distant surgery (especially abdominal), abdominal injury, blood transfusions, intentional or unintentional weight loss, and injury with hematoma formation.
- Alcohol use should be quantified.
- The family history should seek liver disease and jaundice in close relatives.
Physical examination
- Jaundice should be confirmed in good light.
- Dermovascular signs of chronic liver disease should be sought.
- The characteristic facies of Alagille syndrome and its other signs should be looked for in children and young adults.
- The size of the liver, presence of splenomegaly, and ascites.
Laboratory tests
- Full hemogram including red cell indices, and red cell morphology (especially to look for causes of hemolytic anemia, such as spherocytosis, sickling, and spur cells).
- White cell count and differential (including eosinophils), and platelet count.
- The hepatic panel should include both aspartate (AST) and alanine (ALT) aminotransferases, alkaline phosphatase, both total and direct bilirubin, total protein, and albumin. Gamma-glutamyltransferase.
Liver biopsy
- Liver biopsy is used for (intrahepatic cholestasis mainly If we could not reach dx.
- ERCP for extrahepatic cholestasis with the possibility of brush biopsy If suspecting malignancy.
Hepatobiliary imaging
1. Ultrasound
- It differentiates between intra and extra-hepatic cholestasis.
- In extrahepatic cholestasis dilated bile ducts present as a double barrel phenomenon with the diameter of the common bile duct exceeding 8mm.
- In extrahepatic cholestasis, there’s intrahepatic biliary duct dilatation.
- In intrahepatic cholestasis, there’s no intrahepatic biliary duct dilatation.
2. ERCP
The endoscope stops inside the papilla and then we inject urografin to see the bile ducts.
General treatment of cholestasis
- If there’s biliary obstruction, we must relieve the biliary obstruction by any means. If stone = stone extraction.
- If it’s intrahepatic cholestasis we must treat the hepatocellular level disorder.
- Cholestasis whether of intra-hepatic or extra-hepatic origin should be managed along the same general lines.
Nutrition
a) Calorie intake should be maintained and protein must be adequate.
- Neutral fat should be restricted to 40 g daily.
- Additional fat is supplied by medium-chain triglycerides (MCT) which are digested and absorbed quite well into the portal vein as free fatty acids, in the absence of bile salts.
- They can be given as Protagen (Mead-Johnson) or as MCT (coconut oil) for cooking or in salads.
b) In chronic cases, fat-soluble vitamins (A, D, K) are necessary and must be given parenterally.
Management of chronic cholestasis
- Dietary fat: Low neutral fat (less than 40 g). Add medium chain triglyceride, 40 g daily.
- Intramuscular vitamins (every 4 weeks): (In case of severe vitamin deficiency), A 100 000 i.u., D 100 000 i.u., and KI 10 mg.
- Extra defatted milk. Calcium, If bone pain, calcium chloride I. V.
- Ultraviolet light.
Treatment of bone changes
- Vitamin D2 (100 000 units intramuscularly) should be given every 4 weeks to patients with chronic cholestasis and jaundice.
- If the serum phosphate level is low, phosphate supplements must be given.
- These should be given on alternate days to calcium so that the formation of calcium phosphate complexes in the gut is prevented.
Treatment of Pruritus
A) Biliary drainage
Pruritus can be relieved in patients with biliary obstruction by external or internal biliary drainage. The itching disappears or is much improved after 24-48 hours.
B) Cholestyramine (bile acid-binding resin)
This resin will stop itching in 4-5 days in patients with partial biliary obstruction, It is known to bind bile salts in the intestines so eliminating them in the feces, One sachet should be given before and one after breakfast so that the arrival of the drug in the duodenum coincides with gallbladder contraction.
C) Naloxone
An opiate antagonist is being evaluated. It must be given by injection.
D) Anti-histamines
These are of value only for their sedative action.
E) Phototherapy
It converts the unconjugated bilirubin into the photo isomer which can be excreted by the kidney, Ultraviolet radiation, 9-12 minutes daily, may relieve pruritus and decrease pigmentation.
F) Plasmapheresis
This has been used to treat intractable pruritus associated with hypercholesterolemia and xanthomatous neuropathy.
G) Steroids
Glucocorticoids will relieve itching, but at the expense of severe bone thinning particularly in post-menopausal women. Methyltestosterone 25 mg sublingually daily relieves itching within 7 days and is appropriate for mem.
H) Ursodeoxycholic acid
May be effective by reducing toxic bile salts.
I) Rifampicin
Rifampicin (300-450 mg daily) relieves pruritus within 7 days, This may be by enzyme induction or by inhibition of bile acid uptake.
J) Hepatic transplantation
May be the only answer for some patients with chronic, intractable pruritus.
K) Antibiotics
It’s crucial for patients with cholestasis because when there’s biliary obstruction, there’s high susceptibility for secondary bacterial infections, May be indicated for febrile cholangitis but only temporary benefit. It is given in the presence of continued biliary obstruction.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Liver Cholestasis types, causes, features, symptoms, diagnosis, and treatment
Conjugated hyperbilirubinemia cause, symptoms and treatment
Unconjugated hyperbilirubinemia causes, symptoms, diagnosis and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Interventional radiology types, Robotic endovascular systems advantages & disadvantages