Delirium causes, types, diagnosis, treatment, Why do people get delirium and can delirium be cured?
Delirium is an acute, fluctuating, disturbance in mental function characterized by confusion, disorientation, impaired attention, and changes in consciousness. It is a medical condition that results from underlying causes like infections, medications, metabolic imbalances, or substance withdrawal. Delirium is a serious condition, especially in older adults, and can lead to long-term cognitive impairment if not treated promptly.
Delirium
Delirium is an acute, fluctuating syndrome of altered attention, awareness, and cognition. (considered a geriatric emergency), It is an acute disorder of attention and cognitive function. Delirium is the most frequent complication of hospitalization among the elderly and a potentially devastating problem.
Epidemiology
The overall prevalence of delirium in the community is just 1-2%, but in the setting of general hospital admission, this increases to 14-24%.
Characteristics of Delirium
- Delirium develops over a few hours to days, in contrast to conditions like dementia, which progress slowly over months or years.
- Symptoms of delirium fluctuate during the day, with periods of lucidity alternating with confusion. Symptoms are worse at night, a phenomenon known as “sundowning.”
- People with delirium have trouble maintaining focus, thinking clearly, and following conversations. Memory, language, and judgment may be impaired.
- Delirium can range from hyperactivity (agitation and restlessness) to hypoactivity (drowsiness or lethargy), or a mixed form where both symptoms alternate.
- Individuals may experience disorganized or illogical thoughts, and their speech can become incoherent or rambling.
- Visual or auditory hallucinations, as well as delusions (false beliefs), are common.
- Delirium may cause rapid mood swings, anxiety, fear, irritability, or even depression.
Causes of Delirium
- Delirium is caused by a combination of factors, including physical illnesses, metabolic disturbances, medications, and environmental changes, Common causes include:
- Urinary tract infections (UTIs), pneumonia, sepsis, or other infections can trigger delirium, particularly in elderly individuals.
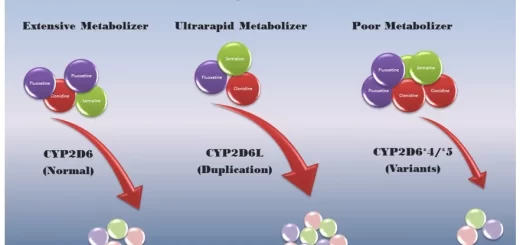
- Certain drugs, especially sedatives, narcotics, anticholinergics, and those used for treating mental health conditions, can induce delirium. Polypharmacy (use of multiple medications) in older adults is a significant risk factor.
- Imbalances in sodium, potassium, or calcium can disrupt brain function and lead to delirium.
- Delirium tremens is a severe form of delirium associated with alcohol withdrawal. Drug intoxication or withdrawal from substances like opioids, benzodiazepines, or recreational drugs can also cause delirium.
- Conditions like liver or kidney failure, hypoxia (low oxygen levels), and malnutrition can contribute to delirium.
- Postoperative delirium is common, especially in older adults undergoing major surgeries, such as hip replacements or cardiac surgeries.
- Prolonged sleep disturbances, often seen in hospital settings, can trigger delirium in vulnerable individuals.
- Head trauma, strokes, or brain infections like encephalitis can cause delirium.
Types of Delirium
There are three main types of delirium, based on the psychomotor activity observed:
- Hyperactive Delirium is characterized by agitation, restlessness, rapid mood swings, and hallucinations. Individuals may become aggressive or hyperalert.
- Hypoactive Delirium: The person may seem withdrawn, drowsy, or lethargic. This form is often missed because symptoms are less obvious, but it is equally dangerous.
- Mixed Delirium involves both hyperactive and hypoactive symptoms that fluctuate over time.
Diagnosis of Delirium
- Diagnosis is clinical and involves recognizing the sudden onset of confusion or changes in mental status. Tools used include:
- Confusion Assessment Method (CAM): A widely used tool to assess the presence of delirium, which focuses on acute onset, inattention, disorganized thinking, and altered consciousness.
- Assessing medical history, medication review, and performing a physical examination to identify underlying causes.
Cognitive Tests: Simple tests to assess attention, memory, and awareness. - Blood tests, urinalysis, and imaging studies (CT scan or MRI) may be done to rule out infections, metabolic imbalances, or brain-related causes.
Treatment of Delirium
Treating delirium involves addressing the underlying cause and providing supportive care, Key aspects include:
- Identifying and treating the cause.
- Administering antibiotics for infections such as UTIs or pneumonia.
- Reducing or stopping medications that may be contributing to delirium.
- Correcting dehydration and nutritional deficiencies (like electrolytes or vitamin B12).
Predisposing factors
- preexisting cognitive impairment or dementia.
- Severe underlying illness.
- High levels of co-morbidity as ischemic heart disease, heart failure hypertension, and diabetes.
- Functional impairment.
- Advanced age.
- Chronic renal insufficiency.
- Dehydration.
- Malnutrition.
- Vision or hearing impairment
- Delirious patients commonly have evidence of underlying chronic brain disease, particularly that associated with cognitive impairment such as Alzheimer’s disease, Parkinson’s disease, cerebrovascular disease, and space-occupying lesions.
- Medications, the most common remediable cause of delirium, contribute to delirium in 40% of cases.
- Insufficiency or failure of any major organ system, esp. kidney and liver failure.
- Hypoxemia and hypercarbia.
- Acute myocardial infarction or H.F
- Occult infection is a particularly notable cause of delirium.
- A variety of metabolic disorders may contribute to delirium including: hypernatraemia or hyponatraemia, hypercalcemia, acid-base disorders, hypoglycemia and hyperglycemia, and thyroid or adrenal disorders.
- Dehydration and volume depletion
- Drug and alcohol withdrawal.
- Environmental factors.
- Psychosocial factors such as depression, psychological stress, pain, or lack of social support.
- Drugs such as antiarrhythmics (quinidine, disopyramide, amiodarone) anticholinergic, antidepressants, antiepileptic, antiParkinson, antihistamines (H1 and H2), aspirin, beta-blockers, barbiturates benzodiazepine, Calcium channel blockers, chemotherapeutic agents, Corticosteroids, digitalis glycosides, non-steroidal anti-inflammatory drugs, opiates and quinolone.
The cardinal features of delirium include:
- acute onset.
- inattention.
- fluctuation.
Work up
- Detailed assessment in search of the predisposing factor-infection, dehydration, electrolyte imbalance, polypharmacy, acute medical illness, a change in therapy, or the destabilization of a chronic condition, visual problems, history of dementia, constipation, and urinary retention.
- Physical examination-infection, volume depletion, abdominal pathology, thyroid disease, anaemia, deep vein thrombosis, and neurological examination.
Investigations
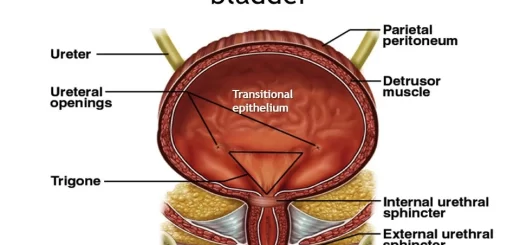
- Infection work-up-Urinalysis and culture.
- Chest x-ray.
- ECG, troponins.
- CBC with differential.
- Electrolytes.
- Liver enzymes, renal functions.
- Thyroid function.
Treatment
- Non-pharmacological (the mainstay).
- Pharmacologic approach: Any drug chosen should be given in the lowest dose for the shortest time possible. Neuroleptics are preferred Haloperidol is the drug of choice. Haloperidol causes fewer side effects.
The recommended starting dose is 0.5 to 1 mg of haloperidol orally or parenterally, repeated every 30 min after the vital signs have been rechecked until sedation has been achieved. The endpoint should be an awake but manageable patient.
A total loading dose of no more than 3 to 5 mg of haloperidol. Subsequently, a maintenance dose consisting of half of the loading dose should be administered within divided doses over the next 24 hours, with the dose tapering over the next few days as the agitation resolves.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Aging and cognition, Dementia symptoms, types, What comes first, dementia or Alzheimer’s?
Causes of Falls in the elderly, How to prevent falls and Why the Elderly die after a fall
Urinary incontinence in elderly causes and treatment, How to correct urinary incontinence?
Properties of cardiac muscles, Cardiac automaticity, and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure, and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk, and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart and Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function