Conjugated hyperbilirubinemia cause, symptoms and treatment
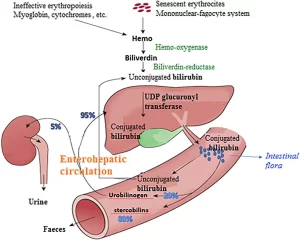
Jaundice is a yellow discoloration of the skin and eyes caused by hyperbilirubinemia, The serum bilirubin level required to cause jaundice varies with skin tone and body region, Conjugated hyperbilirubinemia is a measure of direct reacting bilirubin of >1.0 mg/dL, when the total serum bilirubin (TSB) is ≤5.0 mg/dL, or more than 20% TSB, It is the biochemical marker of cholestasis and a sign of hepatobiliary dysfunction, Unlike physiologic unconjugated hyperbilirubinemia, known as “physiologic jaundice of the newborn.”
Causes of Conjugated hyperbilirubinemia
1. Diminished bilirubin excretion
A. Dubin-Johnson syndrome
Conjugated bilirubin excretion occurs through a pump. If this pump is defective, we get Dubin- Johnson syndrome. It is recessive autosomal inheritance. Age of onset: 10-30 years of age. Triggering factors: Acute viral hepatitis, Alcohol, and Excessive physical and mental strain.
Pathogenesis: Mutation of the canalicular organic anion transporter/cMOAT (also known as the multidrug resistance-associated protein 2; MRP-2) is responsible for defective excretion of conjugated bilirubin.
Clinical picture
1) Chronic or intermittent jaundice with bilirubin between 2-6 mg/dl, Occasionally hepatosplenomegaly. The oral cholecystogram appears negative.
2) Histologically: Characterized by deposition of brown melanin-like pigment (lipomelanin). The pigment is possibly a polymerization product of catecholamine.
3) Laparoscopically: The liver is blue-green to blue-black, The surface is smooth and shiny with intricate vascular multiplication, and the lymphatic vessel of the capsule can appear more pronounced.
B. (Rotor syndrome)
A conjugated hyperbilirubinemia with bilirubin ranging between 2-5 mg/dl with intercurrent icteric episodes triggered by various stress factors.
Pathogenesis:
- Fault in intrahepatic storage of conjugated organic anions that reflux into plasma.
- The hepatocyte can’t store the conjugated bilirubin, so it refluxes back into the blood.
- The excretion of total coproporphyrin in urine is elevated.
- It differs from Dubin Johnson in that the gall bladder opacifies on cholecystography.
Therapy:
The prognosis is good and no specific treatment is required and avoidance of precipitating factors.
Alagille syndrome
Familial paucity of intrahepatic bile ducts (there’s a marked reduction in the number of intrahepatic bile ducts), is not due to a primary canalicular transport abnormality but rather is related to an autosomal dominant mutation of the Jagged I gene) which encodes a ligand of Notch 1, one of four of a family of transmembrane receptor proteins, It leads to cholestasis.
2. Dysfunction of the hepatocytes
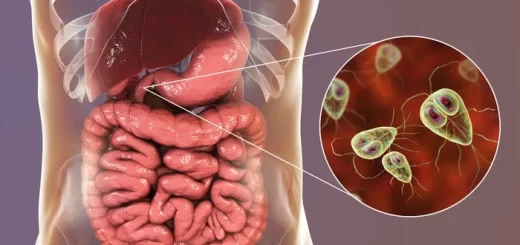
- Acute viral hepatitis.
- Chronic aggressive hepatitis.
- Liver cirrhosis.
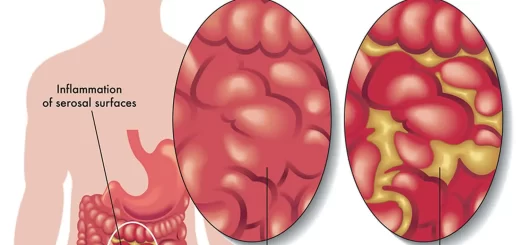
3. Biliary obstruction
- Extrahepatic obstruction (extrahepatic bile ducts).
- Intrahepatic obstruction (intrahepatic bile ducts).
4. Special forms
- Recurrent intrahepatic cholestasis.
- Recurrent cholestasis in pregnancy.
- Recurrent intrahepatic cholestasis of pregnancy.
- Familial intrahepatic cholestasis.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Liver Cholestasis types, causes, features, symptoms, diagnosis and treatment
Unconjugated hyperbilirubinemia causes, symptoms, diagnosis and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Hepatocellular carcinoma symptoms, stages, risk factors, diagnosis, and treatment
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Common procedures of Interventional Radiology and the best Interventional Radiologists