Classification of reflux oesophagitis, Esophageal Manometry and Endoscopic GERD therapy
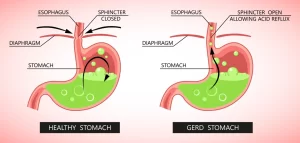
Reflux esophagitis is inflammation of the esophageal mucosa caused by gastroesophageal reflux disease (GERD), which results from the reflux of stomach acid and other gastric contents into the esophagus. It is a common cause of esophageal injury and can lead to complications if untreated.
Reflux Esophagitis
Reflux esophagitis is the inflammation of the esophagus caused by gastroesophageal reflux disease (GERD), where stomach acid and other gastric contents irritate the esophageal lining.
Classification of reflux oesophagitis (Modified) Savary-Miller Classification
- Grade 1: Erythema or diffusely red mucosa oedema causing accentuated fluid loss.
- Grade 2: Isolated round or linear erosions extending from the gastro-oesophageal junction in relation to the folds.
- Grade 3: Confluent erosions extending around the entire circumference or superficial ulceration, but without stenosis.
Ambulatory 24 hr. pH Monitoring
- Physiologic study.
- Quantify reflux in the proximal/distal esophagus: Number of reflux episodes, duration of the longest episode, % time pH<4, DeMeester score.
- Symptom correlation.
Oesophageal pH measurement
- This involves the passage of a fine pH probe into the lower oesophagus, connected to a recording device worn by the patient for 24 hours.
- Measure the duration, frequency, and severity of reflux attacks.
- It is the “gold standard’ of quantifying the degree of reflux.
- Significant acid reflux is diagnosed when the Ph is < 4 for more than 5% of the time (1.2 hour) which is usually taken as an indication for surgical treatment.
Wireless, Catheter-Free Esophageal pH Monitoring
Potential Advantages
- Improved patient comfort and acceptance.
- Continued normal work, activities, and diet study.
- Longer reporting periods possible (48 hours).
- Maintain constant probe position relative to SCJ.
Esophageal Manometry
Limited role in GERD
- Assess LES pressure, location, and relaxation.
- Assist placement of 24 hr.pH catheter.
- Assess peristalsis Prior to antireflux surgery.
- Determine the length and position of the LOS.
- Measures the LOS pressure and length.
- Assessment of oesophageal peristalsis and its propagation.
- Short or weak LOS is a major cause of reflux esophagitis.
- A LOS pressure of <4 mmHg is abnormal and is an indication for surgery, (Normal LOS pressure is (5-30 mmHg).
- Diagnosis of achalasia).
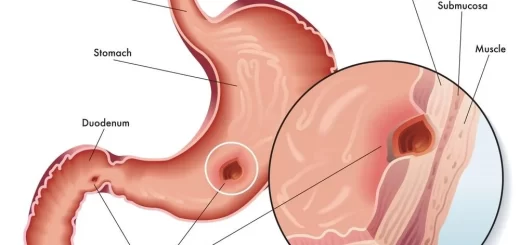
PPIs block the proton pump within the mucosal cells of the stomach lining, thus inhibiting the active transport of hydrogen ions across the membrane and thereby almost completely abolishing gastric acid production. Their clinical effect is better than H2-receptor antagonists, leading to better acid suppression and more effective symptom control and healing of ulcerative esophagitis in most patients. A full-dose therapy should be started until the esophagitis has healed, followed by long-term maintenance therapy using a reduced (usually half-strength) dose.
Recently, a more powerful second-generation PPI has also been introduced. Esomeprazole is the s-isomer of Omeprazole & has even greater & more long-lasting anti-secretory activity. At present, it is largely used in more severe diseases (grades III and IV) or as 2nd-line treatment where_first generation’ PPIs failed to control symptoms.
Mucosal protection agents e.g. Sucralfate help to protect against other (non-acidic) agents in the refluxate. However, sucralfate has an unpleasant taste and may produce constipation.
Prokinetic agents e.g. Metoclopramide, Domperidone, and Erythromycin, improve gastric emptying and clearance of contents from the lower esophagus, but are of little benefit in the treatment of reflux esophagitis.
Eradication of H. pylori infection: There is little evidence that this is of any benefit in the treatment of reflux esophagitis and is not currently recommended as standard treatment.
Treatment Modifications for Persistent Symptoms
- Improve compliance.
- Optimize pharmacokinetics.
- Adjust the timing of medication to 15-30 minutes before meals (as opposed to bedtime).
- Allows for high blood levels to interact with the parietal cell proton pump activated by the meal.
- Consider switching to a different PPI.
GERD is a Chronic Relapsing Condition
- Esophagitis relapses quickly after cessation of therapy: 50% relapse within 2 months, 80% relapse within 6 months.
- Effective maintenance therapy is imperative.
When to Discuss Anti-Reflux Surgery with Patients
- GERD requiring long-term PPI-BID in a healthy young patient.
- Persistent regurgitation/aspiration symptoms.
- Intractable GERD – rare: Difficult to manage strictures, Severe bleeding from esophagitis, Non-healing ulcers, and Barrett’s esophagus.
Indications of Surgical Treatment
Antireflux surgery
- Patient preference
- Failed medical management.
- GERD.complications.
- Atypical symptoms with reflux documented on 24-hour pH monitoring.
- Medical complications attributable to a large hiatal hernia.
Tenets of surgery:
- Restore intra-abdominal length of oesophagus.
- Reduce hiatal hernia.
- Repair diaphragm.
- Strengthen GE junction.
Strengthen antireflux barrier via gastric wrap 75-90% effective at alleviating symptoms of heartburn and regurgitation.
Advantages of surgery
- Anti-reflux surgery is the most effective long-term treatment for GERD as it prevents the reflux of all gastric contents.
- Surgery also avoids the problem of poor patient compliance with long-term medication.
Side-effects of surgery:
Dysphagia (usually short-lived), inability to belch, the so-called gas bloat syndrome and excessive flatus.
Types of anti-reflux surgery
- Trans-abdominal and trans-thoracic approaches.
- Both can be performed through either open or minimal access (laparoscopic/thoracoscopic) techniques.
1. Nissen fundoplication (360-degree):
The “gold standard’ operation, in which the fundus of the stomach is wrapped completely around the lower oesophagus, following a hiatal repair.
Complication: dysphagia and gas bloat.
- Dissection of the fundus of the stomach by cutting the short gastric vessels plus separating it from the spleen.
- Dissection of the crura.
- Bringing the lower oesophagus to the stomach.
- Hernia repair.
- Fundoplication.
2. Partial fundoplication:
- In an attempt to ↓ dysphagia, various partial fundoplications have been described.
- The rationale behind these procedures is to create a sufficient wrap to prevent reflux but not so tight.
- The major modifications in use are the Lind (270o), anterior partial (e.g. Watson), posterior partial (e.g. (Toupet), and sub-total fundoplications. Although the use of a partial fundoplication may ↓ the risk of dysphagia, concerns have been expressed over the long-term durability of these procedures.
3. Other less common trans-abdominal approaches:
- They include the Hill posterior gastropexy and Collis-gastroplasty.
- The latter is particularly useful in patients in whom the gastroesophageal junction (GEJ) cannot be reduced below the diaphragm.
4. Trans-thoracic approach:
- The most common is the Belsey Mark IV procedure.
- Here the lower esophagus is mobilized up to the level of the aortic arch and is then sutured to the gastric fundus and the diaphragm, to ↓ any hiatus hernia & wrap the fundus over the front of the esophagus.
Results (outcome) of surgery
- Anti-reflux surgery produces effective symptom control in 85-90% of patients.
- The major side effects include persistent heartburn (5-8%), dysphagia (3-8%), gas bloat, and inability to belch and/or vomit.
- Other less common complications include esophageal perforation, pneumothorax, chest infection, splenic damage, and deep vein thrombosis (DVT).
Endoscopic GERD therapy
- Radiofrequency energy delivered to the LES (Stretta procedure).
- Suture ligation of the cardia (Endoscopic plication “bard endoCinch”).
- Submucosal implantation of inert material in the region of the lower esophageal sphincter (Enteryx).
- Linx system.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
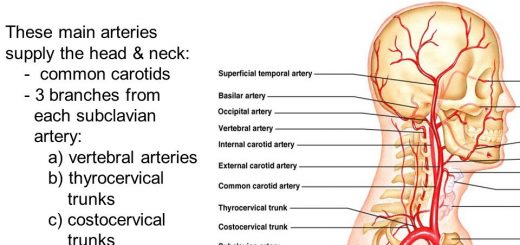
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion