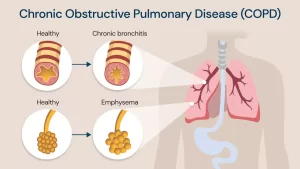
Chronic Obstructive Pulmonary Diseases Treatment, Types and Causes of COPD
Chronic obstructive pulmonary disease (COPD) is a group of lung diseases that block airflow and make breathing difficult, Emphysema and chronic bronchitis are two conditions that makeup COPD.
Chronic obstructive pulmonary diseases
Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases and influenced by host factors including abnormal lung development, Exacerbations and comorbidities contribute to the overall severity in individual patients.
Etiology & Risk Factors
- Smoking (the most important risk factor), it causes: Submucosal bronchial gland hypertrophy and goblet cell hyperplasia → mucous hypersecretion, Impairment of muco-ciliary function, Airway neutrophilic infiltration, Protease antiprotease imbalance, Oxidant antioxidant imbalance (Cigarettes contain many free oxygen radicals resulting in oxidative stress to the lungs. Also, the serum concentration of antioxidants is less in cigarette smokers), Increases frequency of respiratory infections.
- Environmental or occupational exposure: biomass fuel combustion, coal mines, cotton industries.
- Gender: Males were more susceptible than females (Recently, COPD is almost equally prevalent in males and females).
- Genetic factors: alpha 1 antitrypsin deficiency (MTD), especially the homozygous form (the most common genetic factor).
- Recurrent bronchopulmonary infections in early childhood.
Pathology
Patients with COPD have an enhanced or abnormal response to inhaled toxic agents. This amplified response may result in:
- Large airway inflammation → Chronic bronchitis and mucous hypersecretion.
- Small airway inflammation → Bronchiolitis.
- Lung parenchyma destruction Emphysema.
Chronic bronchitis
It is defined in clinical terms as the presence of cough and sputum production for most days for at least 3 months for 2 consecutive years when other causes as bronchiectasis and TB are excluded, Chronic bronchitis results from an innate immune response to inhaled toxic particles and gases, particularly tobacco smoke.
Pathology
Excessive mucus secretion in chronic bronchitis results from the increase in the size and number of mucus-secreting glands, There is an increased ratio of mucus glands to wall thickness (Reid index), Normal 40%, but in COPD, up to 70%.
Emphysema
It is a disease of the lung parenchyma characterized by abnormal, permanent enlargement of the airspaces distal to the terminal bronchiole, accompanied by destruction of their walls, “true emphysema”, When dilatation of airspaces occurs without destruction, it is called “false emphysema”.
Pathology
The enlargement of the air spaces distal to the terminal bronchioles and destruction of the alveolar walls.
Types of emphysema include:
The site of destruction within the acinus (terminal respiratory unit) is the basis for the classification of emphysema.
- Centri-acinar or centri-lobular emphysema: the central part of the acinus is involved, and usually occurs in association with smoking and chronic bronchitis affecting mainly upper lung zones.
- Pan-acinar pan-lobular emphysema: all acinus is or involved uniformly, usually occurs in association with MTD, affecting mainly lower lung zones. And is seen in patients with alpha 1- antitrypsin (AAT) deficiency.
Phenotypes
- Type A COPD (Pink Puffer): characterized by emphysema.
- Type B COPD (Blue Bloater): characterized by chronic bronchitis.
- Mixed type COPD: most common.
Clinical Picture
The patient is usually a male, chronic heavy cigarette smoker & above 50 years of age.
1. Symptoms
- Prolonged history of chronic cough with mucoid or mucopurulent expectoration. Cough often presents only at first, later on, cough occurs throughout the day (may be attributed by the patient to “smoker’s cough”).
- Dyspnea with wheezing. Dyspnea is gradual slowly progressive over the years occurring initially on exertion but later at rest. Wheezing is usually persistent or continuous (not in attacks as bronchial asthma).
- Chest pain may occur due to: Chronic cough causing strain of intercostal muscles. Rupture of emphysematous bullae causing pneumothorax. Complicating pneumonia-causing pleurisy.
- In advanced COPD cases: Manifestations of respiratory failure, Lower limb oedema: due to corpulmonale, salt and water retention, Muscle wasting and weight loss.
II. Signs
Chest examination:
A. Manifestations of hyperinflation:
1. Inspection
- Increased antero-posterior diameter or barrel-shaped chest if: Horizontal ribs, Wide intercostal spaces, Wide subcostal angle, Kyphoscoliosis.
- Bilateral limitation of chest movement.
- Costal margin retraction on inspiration (Hoover’s sign).
- Weak or absent cardiac pulsations.
- Epigastric pulsations (also may be present due to right ventricular enlargement).
2. Palpation
- The trachea is central, Bilateral limitation of chest expansion.
- TVF is decreased bilaterally.
3. Percussion
Hyperresonance with encroachment on cardiac & hepatic dullness.
4. Auscultation
- Diminished vesicular breath sounds with prolonged expiration (harsh vesicular).
- Distant heart sounds
- Generalized wheezes (rhonchi).
- Early inspiratory crepitation.
B. Signs of respiratory failure
- Hypoxemia: Central cyanosis,
- Hypercapnia: CO2 narcosis
- Drowsiness & hypersomnia.
- Asterixis (flapping tremors).
- Increased intracranial tension & papilledema.
- Coma occurs terminally.
Complications
- Acute exacerbations.
- Acute Respiratory failure.
- Pneumonia.
- Car pulmonale & right-sided heart failure.
- Pneumothorax.
- Bronchial obstruction & collapse.
- bronchiectasis.
- Erythrocytosis.
- Thromboembolism.
- Salt & fluid retention.
- Complications of chronic cough.
Investigations
1. Chest X-ray:
Signs of hyperinflation:
- Lung hyper translucency.
- Transverse ribs with wide intercostal spaces.
- Low flat diaphragm.
- Elongated (ribbon-shaped) cardiac shadow.
- Tenting (cupping) of the diaphragm (sure sign of hyperinflation).
- Increased retrosternal air in lateral view (sure sign).
- Emphysematous bullae may be present → large air-fluid space (cyst) (sure sign).
- Accentuation of pulmonary vessels near the hilum (sure sign).
2. CT chest: the best method to detect the severity of emphysema.
3. Pulmonary function tests:
A. Ventilation tests: (Spirometry)
- FEVI & PEFR are decreased.
- Forced vital capacity (FVC) is decreased.
- Decreased FEV1/FVC ratio <0.7.
- Residual volume (RV) and total lung capacity (TLC) are increased.
- Maximum breathing capacity (MBC) is markedly reduced.
- Reversibility test (change in FEVI after bronchodilator inhalation): absent or less than 12%.
4. ABG changes: Chronic hypoventilation: ↓ PO2, ↑ PCO2, ↑ HCO3.
5. Sputum culture and sensitivity: may detect organisms, especially pneumococci & H. influenza.
6. CBC: polycythemia.
7. AAT level: in cases with AATD.
Management of COPD
- Treatment of stable COPD patients.
- Treatment of acute exacerbations.
- Treatment of acute respiratory failure on top of COPD.
A. Treatment of stable COPD patients (outpatient treatment)
- Prevention: Smoking cessation and/or nicotine replacement by patches or gums. Reduce or prevent air pollution. Pneumococcal or influenza vaccination.
- Pulmonary rehabilitation: education, exercise, and physiotherapy.
- Long-term oxygen therapy (LTOT).
- Pharmacological therapy.
- Alpha 1 antitrypsin replacement therapy.
6. Interventional therapy (Surgical).
B. Treatment of acute exacerbations (Inpatient treatment):
- Treatment of Infection by empirical antibiotic therapy (amoxicillin- clavulanic acid, macrolide, fluroquinolone, or 2nd generation cephalosporine) for 5 to 7 days. Empirical therapy is started till the results of sputum culture and sensitivity testing for modification of antibiotic therapy.
- Systemic steroids: IV steroids equivalent to 40 mg prednisone per day for 5 days ± ICS.
- Bronchodilators: Inhaled SABA with/without SAMA using a nebulizer.
- Mucolytics: N-acetyl cysteine or erdosteine or bromhexine hydrochloride (bisolvon).
- Management of superadded complications: e.g., pneumothorax, myocardial ischemia, pulmonary embolism, arrhythmias.
- Expectorants e.g. potassium iodide.
In both outpatient and inpatient treatment of COPD, dyspneic patients should be given a trial of bronchodilators even if pulmonary function testing shows that they do not manifest significant bronchodilation, because bronchodilator responsiveness may vary over time.
Pharmacological treatment ENTAILS
1. Bronchodilators (cornerstone in treatment):
a) Beta 2 Agonists: first line:
- Short-acting beta 2 agonists (SABA): salbutamol (albuterol).
- Long-acting beta 2 agonists (LABA): salmeterol, formoterol.
b) Muscarinic antagonists
- Short-acting muscarinic antagonists (SAMA): ipratropium bromide.
- Long-acting muscarinic antagonists (LAMA): tiotropium (reduces exacerbations).
c) Theophylline:
- Bronchodilator + anti-inflammatory effect + enhances respiratory muscle function.
- It is not widely used given its narrow therapeutic range and severe cardiac and neurological adverse effects.
3. Anti-inflammatory agents (beneficial for patients with frequent exacerbations).
Corticosteroids:
- Given the underlying pathophysiology of emphysema, corticosteroids would be expected to provide little benefit, because tissue destruction is the basic disease mechanism.
- Only some patients derive significant benefit from corticosteroids.
- It is used as Inhaled corticosteroids (ICS) by inhaler or nebulized nebules, and Systemic IV steroids in acute exacerbation of COPD.
- Preparations: Beclomethasone, budesonide, or fluticasone by inhalation. Prednisone 20-40 mg/d orally with rapid tapering after improvement.
3. Mucolytics and antioxidant agents (erdosteine, N-acetyl cysteine
Oxygen therapy
It is the long-term continuous administration of low-flow O2 at home.
It is indicated in cases of severe hypoxia:
PaO2 < 55 mm Hg or SaO2 <88%.
PaO2 56 mmHg to 59 mm Hg or SaO2 89% if there is (i.e. plus evidence of):
- Corpulmonale (P pulmonale by electrocardiogram).
- Polycythemia (hematocrit 2: 55%).
- Congestive heart failure.
Goal PaO2 = 60 mmHg, SaO2 = 90-92%.
Methods of administration: nasal prongs or mask.
Domiciliary 02 via compressed O2 in cylinders, and O2 concentrators.
Rate: 1-3 L/min.
Low-flow oxygen (1-3 L/min) via nasal cannula or face mask is used in COPD patients.
High-flow oxygen is avoided in COPD patients, this is based on the fact that the respiratory drive in COPD patients is initiated by hypoxia rather than hypercapnia. Therefore, correcting hypoxia will abolish the patient’s respiratory drive resulting in apnea and further hypoventilation.
Value of long-term oxygen therapy (LTOT): It improves
- Symptoms.
- Pulmonary hypertension.
- Polycythemia.
- Arrythmias.
- Exercise intolerance.
- Quality of life and survival.
Interventional therapy:
- Bullectomy.
- Lung volume reduction surgery.
- Bronchoscopic lung volume reduction.
- Lung transplantation.
B. Management of acute respiratory failure
If acute exacerbation of COPD is not adequately treated, it can lead to acute respiratory failure (ARF). ARF is defined as failure of the respiratory system to supply sufficient oxygen to the blood and body organs with or without failure of adequate ventilation i.e. CO2 wash.
A. Acute type I respiratory failure (Hypoxemia Or Non-hypercapnic ARF)
- Showing only hypoxemia without hypercapnia and is usually due to pulmonary causes only.
- Hypoxemia PO2 <55-60 mmHg.
- Managed by oxygen therapy administered via nasal cannula, face mask or venturi mask (controlled/fixed oxygen therapy).
- Supplemental oxygen should be titrated to improve the patient’s hypoxemia with a target SaO2 of 88-92% (PO2 55-60 mm Hg).
B. Acute type II respiratory failure (Hypercapnic ARF)
Showing hypoxemia, hypercapnia, and respiratory acidosis).
This type can be due to pulmonary causes such as COPD and extrapulmonary causes such as brain lesions or neuromuscular junction disease.
Hypoxemia PO2 < 55-60 mmHg + hypercapnia (PCO2 > 45 mmHg) + respiratory acidosis (pH < 7.35).
Managed by either non-invasive pressure ventilation (BIPAP) or invasive mechanical ventilation (Intubation + mechanical ventilator).
If the patient is on 02 therapy, then ARF is monitored by an oxygenation index. This is a ratio of arterial 02 tension and inspired O2 fraction or concentration. If it is < 200, this diagnoses ARDS, and if less than 150, ALI is diagnosed.
Factors improving survival in COPD
They alter the natural history of the disease favorably:
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Steps of Asthma control, What is good control of asthma? and What is asthma management?
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax