Chronic Low Back Pain diagnosis, symptoms, treatment and Seronegative Spondyloarthritis types
Chronic back pain is defined as pain that occurs > 3 months, Identifying back pain as acute or chronic is one of the key processes in determining the source of the pain, It is important to distinguish inflammatory from mechanical back pain as early as possible as the management and treatment of the two conditions is very different.
Differential diagnosis of low back pain
Possible causes of mechanical back pain include:
- Lumbar disc prolapse.
- Degenerative disc diseases.
- Facet joint derangement.
- Osteoarthritis.
- Muscle imbalance.
- Spinal stenosis.
- Herniated disc.
- Osteoporotic compression fracture.
- Spondylolisthesis.
- Traumatic fracture.
- Severe kyphosis.
- Severe scoliosis.
- Transitional vertebrae.
Possible causes of inflammatory back pain include:
- Axial spondyloarthritis.
- Psoriatic arthritis (PSA).
- Inflammatory bowel disease.
- Non-radiographic axial SpA.
- Undifferentiated spondyloarthritis.
- Enteropathic.
- Juvenile spondyloarthritis.
- Acute anterior uveitis.
Other possible causes of back pain include:
- Abdominal aortic aneurysm.
- Tumours including metastases.
- Renal diseases.
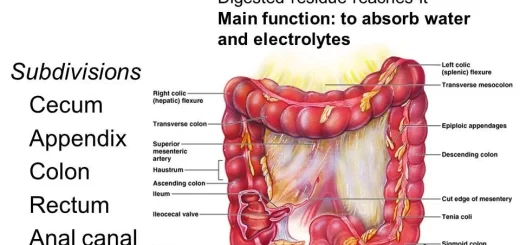
- Gastrointestinal diseases
- Infections such as: Epidural abscess, Osteomyelitis, Septic discitis, Paraspinous abscess, and Shingles.
- Disease of the pelvic organs.
- Fibromyalgia
- Paget’s disease of bone.
- Scheuermann’s disease (osteochrondrosis).
- Tuberculous sacroiliitis.
- Depression.
Infections that result in back pain due to inflammatory sources can also lead to mechanical pain as a result of changes caused by the infection, for example, disc degeneration and collapse resulting from vertebral disc infection.
Comparison of Mechanical back pain (MBP) vs. Inflammatory back pain (IBP):
MBP:
- Age of onset: any age.
- Variable onset; may be acute.
- Pain may worsen with movement.
- Pain often improves with rest.
- Morning stiffness < 30 minutes.
IBP:
- Age of onset 40 years.
- Insidious onset, less likely to be acute.
- Pain improves with exercise.
- Pain does not improve with rest.
- Pain at night which may wake the patient during the second half of the night.
Inflammatory Back Pain
- If you suspect your patient may be suffering from IBP, there are several key questions you can ask to help further classify if it is mechanical or inflammatory in nature.
- The following 5 questions are from the ASAS (Assessment of SpondyloArthritis International Society) criteria for identifying inflammatory back pain.
- Inflammatory back pain requiring further investigation is usually indicated if the answer is ‘yes’ to 4 or more of these parameters.
ASAS (Assessment of Spondylarthritis International Society) criteria
- Did your back pain start when you were aged younger than 40?
- Did your back pain develop gradually?
- Does your back pain improve with movement?
- Do you find there is no improvement in your back pain when you rest?
- Do you suffer from back pain at night which improves upon getting up?
In addition to the key distinguishing features, as outlined by the ASAS criteria for inflammatory back pain to the left, other signs of Inflammatory back pain to look out for include:
- Good response to NSAIDs.
- Alternating buttock pain.
- Waking during the second half of the night because of back pain.
- “Morning stiffness” pain and stiffness for > 30 minutes after rising in the morning.
During physical examination, there are several key features to be aware of which may indicate inflammatory back pain:
- Observed postural changes.
- Tenderness over enthesis sites.
- Loss of hip abduction.
- Reduction of the range of movement in the lumbar spine.
- Pain or tenderness over the sacro-iliac joint, lumbar spine and/or thoracic spine.
Who to refer to?
Once you have established if the back pain is mechanical or inflammatory you can then refer to the patient to the appropriate service:
- Mechanical Back Pain: If MBP is suspected refer to local musculoskeletal interface service (or appropriate secondary care service)
- Inflammatory Back Pain: If IBP is suspected refer to Rheumatology (or back to the GP to refer appropriately).
Seronegative Spondyloarthritis
It is a heterogenous interrelated group of diseases sharing genetic immunological, clinical, and imaging features:
- Absence of rheumatoid factor.
- Axial arthritis including spondylitis and sacroiliitis.
- Peripheral inflammatory oligo-arthritis.
- Enthesitis, dactylitis.
- Extra-articular manifestations.
- Overlap among the various diseases.
- The tendency towards familial aggregation.
- Presence of HLA-B27.
Classification Of Spondyloarthritis (SpA)
- Ankylosing spondylitis (AS).
- Non-radiographic axial SpA (nr-axSpA).
- Undifferentiated spondyloarthritis (UspA).
- Reactive arthritis (formerly called Reiter syndrome).
- SpA associated with psoriasis or psoriatic arthritis.
- SpA-associated with Crohn’s disease and ulcerative colitis.
- Juvenile onset spondyloarthritis.
- Acute anterior uveitis.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)