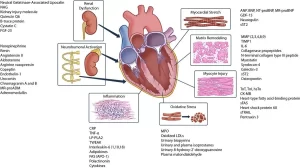
Cardiac Markers review, definition, list, test, and myoglobin function
Myoglobin is a low-molecular-weight haem-containing protein. Found in both skeletal and cardiac muscle. Due to its low molecular weight, it is rapidly released from the myocardium upon damage. A typical rise occurs within 2-4 hours after the onset of acute myocardial infarction. This is useful for the early diagnosis of acute myocardial infarction.
Myoglobin
Unfortunately, myoglobin is not cardiac specific, being also found in skeletal muscle, and thus is less useful in the diagnosis of acute myocardial infarction unless used in conjunction with other markets.
Creatine kinase and CK-MB isoenzyme
Creatine kinase acts as a regulator of high-energy phosphate production and utilization within contractile tissues. Cytoplasmic CK is a dimer, composed of M and/or B subunits, which associate forming CK-MM, CK-MB, and CK-BB isoenzymes.
CK-MM is the main isoenzyme found in striated muscle. CK-MB is found mainly in cardiac muscle Trace amounts of CK-MB are found in skeletal muscle. CK-BB is the predominant isoenzyme found in the brain, colon, ileum, stomach, and urinary bladder.
Serum total CK activity and CK-MB concentration rise in parallel following myocardial injury, starting to increase 4-6h after injury, reaching peak serum concentrations after 12-24h and returning to baseline after 48-72h.
Serum CK-MB is more specific for myocardial damage than serum total CK, which may be elevated in many conditions where the muscle is damaged. An increase in CK-MB in the plasma may not be seen until 4-8 h after the onset of chest pain.
When the diagnosis is not obvious, an elevated CK-MB or an increase in CK-MB of more than 15% over a 4-h period, even if both values are within the reference range, are suggestive of myocardial infarction.
The detection of a trend by serial measurements, if feasible, may provide more information than single measurements. If CK does not increase in a patient with chest pain, myocardial infarction is unlikely, a failure of an elevated CK to fall suggests that an extension of the infarct has occurred.
AST and LDH (Lactate Dehydrogenase)
AST and LDH measurements are rarely of practical value in the management of patients with suspected myocardial infarction. Exceptionally, when a patient with chest pain presents late, measurement of LDH may be helpful as this enzyme remains elevated in the plasma for several days following myocardial infarction.
Troponins
Their function is the regulation of striated and cardiac muscle contraction. Three troponins have been reported, namely:
- Troponin C (TnC).
- Troponin I (Tnl).
- Troponin T (TnT).
There are no structural differences between cardiac and skeletal muscle TnC. However, the cardiac and skeletal forms of Tnl and TnT are structurally different and can be distinguished by immunological assays.
Troponin I and TnT appear in the plasma 4-8 hours after symptoms of acute myocardial infarction and are best measured 12 hours after the start of chest pain.
They are therefore not early markers of acute myocardial infarction, but they do stay, elevated for about 7-10 days in plasma, which makes them useful in the late presentation of chest pain.
An increased Tnl or TnT concentration is a sensitive marker of occult myocardial damage even in non-ischaemic conditions. Troponin T may be elevated in patients with chronic renal failure and thus may not be so cardiac-specific.
Ischaemia-modified albumin
A new marker, ischaemia-modified albumin, is raised in the presence of myocardial ischaemia and may be used in the future in conjunction with conventional cardiac markers.
Determination of Lactate Dehydrogenase Activity
Principle:
Kinetic determination of Lactate Dehydrogenase:
LDH catalyzes the following reaction:
LDH
Pyruvate + NADH + H+ → L-Lactate + NAD+
The initial oxidation rate of NADH is proportional to the LDH catalytic activity. LDH activity in the sample is calculated by measuring the per-time absorbance decrease at 340 nm.
Specimen collection:
Serum plasma (Heparin EDTA).
Do not use hemolyzed serum, as red cells contain a high concentration of LDH which can cause falsely positive results. The serum should be separated from the clot as soon as possible. LDH in serum is stable for up to 2-3 days at room temperature (15-25 °C). In order not to compromise the LDH fraction thermal transiency, do not freeze, and do not expose serum to high temperature (+37°C). Shake and bring the samples to room temperature (15-25°C) before using.
Reagent composition
All reagents are stable until the expiration date when stored refrigerated at 2-8 °C. Mix 5 volumes of R1 with one volume of R2. The working solution is stable for 2 months at 2-8°C or for 1 week at 15-25 °C.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Lipid profile test, Hyperlipidemia causes, Cholesterol sources and importance
Blood analysis, Hemolysis, importance, structure, types, and hemolysis test results
Control of insulin secretion, diabetes mellitus, Glucagon, Somatostatin & features of DNES
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Diabetes mellitus symptoms, causes, types, and sources of glucose in the blood
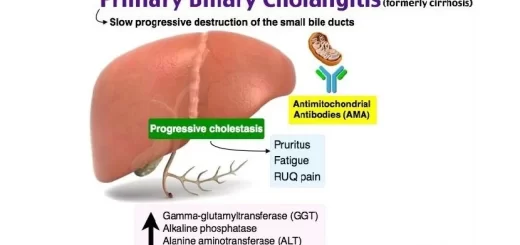
Bile pigments function, names, Cholesterol, Fatty acids, lecithin & Types of jaundice