Bronchiectasis causes, Is a bronchiectasis serious?, What is the best medication for bronchiectasis?
Bronchiectasis is abnormal permanent dilation of the medium-sized bronchi with destruction of bronchial elastic and muscular elements and repeated remission and relapse of bacterial infection.
Bronchiectasis
Bronchiectasis is one of the groups of chronic suppurative lung diseases (other this group include chronic lung abscess and empyema with bronchopleural members of the fistula). Bronchiectasis is classified into congenital and acquired bronchiectasis.
Pathophysiology of Bronchiectasis
Whatever the cause of the obstruction it will accumulate large amounts of Bronchial secretions (which is a good media for recurrent infections that will get more and more secretions) and elastases (breaking the elastic fibers in the bronchi that will decrease the compliance of the bronchial tree). This obstruction causes air tapping and permanent dilatation
- Wall→ thinned.
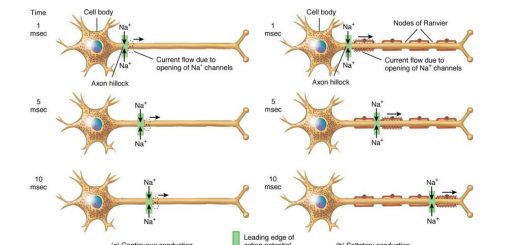
- Cartilaginous rings → Soft or lost epithelium → non-ciliated cells
- Supplying blood vessels→ thrombosed, with abnormal vascular communications (bronchial and pulmonary circulation), this can develop Hemoptysis & Shunt (hypoxia).
Bronchiectasis can be:
1. Acquired
- Atelectasis (Bronchial obstruction): Such obstruction may be: intra-bronchial such as foreign bodies, mucus plug, Post TB stenosis, endo-bronchial obstruction by neoplastic lesion, or extra bronchial compression by enlarged lymph glands or tumor.
- Infection (complicated pneumonia): Although atelectasis leads to infection as previously described, yet infection alone (even without atelectasis) can directly cause bronchiectasis through subsequent fibrosis which exerts traction on the bronchial wall (traction bronchiectasis).
- Acquired immunodeficiency: This causes recurrent infections. It can occur in the acquired immunodeficient syndrome (AIDS), multiple myeloma, chronic lymphatic leukemia, and lymphoma.
2. Congenital
a) Immotile cilia syndrome (Kartagener’s syndrome): which is better called dyskinetic cilia syndrome, it affects respiratory epithelial ciliated cells and spermatozoa. This syndrome is characterized by bronchiectasis, sinusitis or underdeveloped sinuses, male infertility, and dextrocardia with/without situs inversus. The most common pathological abnormality is deficiency of the dynein arms of the respiratory tract cilia spermatozoa as well as of spermatozoa
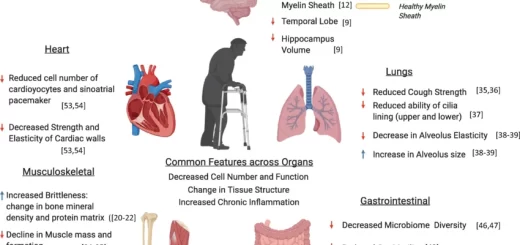
b) Cystic fibrosis (Mucoviscidosis): It is inherited by an autosomal recessive gene that results in a mutation in CEIR protein resulting in abnormal chloride transfer across the cell membrane. It is characterized by high Na+ (>70 mEq/L) and high Cl−(>60 mEq/L) in sweat. It is also characterized by the presence of thick viscid mucous that affects multiple organs resulting in:
- Pulmonary manifestations of cystic fibrosis: Recurrent bronchitis, Bronchiolitis, Atelectasis and Bronchiectasis.
- Intestine: intussusception, meconium ileus (in newborns).
- Pancreas: Diabetes mellitus, Steatorrhea secondary to Pancreatic Lipase Deficiency and pancreatitis.
- Kidney: Amyloidosis.
- Liver and Gallbladder: Biliary cirrhosis and Gall stones.
- Infertility (Sterility): From obstructive azoospermia in males.
c) Macleod’s syndrome: It is a rare lung disorder characterized by a unilateral reduction in the pulmonary vasculature resulting in unilateral emphysema and bronchiectasis.
d) Sequestrated lobe: It is a congenital abnormality by which a portion of the lung (usually of the left lower lobe) becomes isolated i.e. sequestrated from the rest of the lung during development. Occasionally the sequestrated part is not included in the tire lung and in this situation, it is described as extralobar sequestration.
However, The Isolated Segment Is Most Often Included Within the Lower Lobe (Intralobar Sequestration). Infection May Reach It Through the Blood Stream. Once infection occurs communication between such sequestrated lobe and the bronchial tree occurs with recurrent expectoration of such suppurative secretions.
There is always an abnormal blood supply to the sequestrated area, usually from the aorta. Such abnormal blood supply should be demonstrated by angiography and clamped before surgical resection of this sequestrated lobe.
e) Alpha 1 antitrypsin deficiency (AATD): Results in congenital emphysema and bronchiectasis. It is a congenital deficiency of a protective protein that antagonizes the action of protease enzymes released from the rupture of different cells. Such enzymes cause proteolysis of the lung tissues.
f) Congenital immunodeficiency e g., Hypogammaglobulinerua.
g) Young syndrome.
h) Other conditions that are associated with bronchiectasis:
- Disorders of connective tissues eg. Ehlers-Danlos syndrome, Marfan syndrome.
- Tracheobronchomalacia.
- Yellow nail syndrome: syndrome of primary lymphoedema, yellow nails, and pleural effusion.
- Collagenic diseases: as rheumatoid arthritis and systemic lupus erythematosus.
Clinical Picture
Chronic expectoration of large amounts of purulent sputum (yellowish, greenish or bluish) that is usually offensive due to associated anaerobic infections e.g.: by bacteroids. May be blood-tinged sputum or frank hemoptysis.
Bronchiectasis usually affects the basal segments of both lower lobes. However, post-tuberculous bronchiectasis is usually located in the upper lobes. Complications of bronchiectasis include massive haemoptysis, recurrent pneumonia, empyema, lung abscess, and brain abscess.
1) Symptoms
- Cough, expectoration.
- Halitosis.
- Fever.
- Wheezing: Smoking, Bronchitis, Irritants
Cough: either dry or wet:
- Greatest amounts when changing posture.
- Offensive odour.
- Purulent sputum.
- ↑amount>300 cc (exacerbations).
Dry cough and the only presentation is hemoptysis “Bronchiectasis hemorrhagica sicca”, Seen in post tuberculous infection in upper lobes. These zones are kept dry (Sicca) because of their good drainage. Dyspnea and toxemia depend on the extent of bronchiectasis.
Massive haemoptysis.
→Fatal
→Come from a systemic source (bronchial artery). Recurrent haemoptysis is one of the features of presentation so the disease must be listed among the D.D. of haemoptysis.
2) Signs
■ General: Wt loss, emaciation clubbing, cyanosis dyspnea.
■ Local:
- If chest deformity→ prolonged course.
- Limited chest expansion, and retraction.
- Localized rhonchi, persistent crepitations even in the asymptomatic patients (lower lobes) Sometimes mediastinal shift.
Criteria for diagnosis
- Chronic daily productive tenacious, foul smell layers) cough lasting (mucopurulent, sputum settling into months to years.
- plus, compatible findings on high-resolution CT.
Investigations
1. CXR: reveals the presence of:
- Microcystic shadows i.e. honeycomb appearance.
- Atelectasis-crowding rib.
- Fibrous bands.
2. Bronchogram (Obsolete) is made by passing a catheter in the tracheobronchial tree and then injecting a radio-opaque dye. (Not used nowadays).
Bronchiectasis is classified pathologically into:
- Cystic (saccular) bronchiectasis which ends by blind sacs. This type usually has the worst prognosis. massive hemoptysis can occur from angiomatoids which are the site of intrapulmonary shunts.
- Cylindrical bronchiectasis.
- Fusiform (varicose-like) bronchiectasis with areas of constrictions.
3. Lab investigations:
- Leukocytosis with neutrophilia → acute exacerbation.
- Lymphocytosis→ chronic infection.
- Polycythemia in advanced cases is secondary to hypoxia.
- Sputum for culture and sensitivity and also to exclude TB. if bronchiectasis is present in the upper lobes.
4. Chest high-resolution CT (HRCT): the most important diagnostic modality. It has now replaced previous obsolete methods such as bronchogram. In HRCT scan bronchiectasis appears as microcystic shadows i.c.. honeycomb appearance.
5. Pulmonary function tests (PFT): mixed obstructive and restrictive pattern.
- Obstructive pattern: ↓ FEV1, FEV1 %
- Restrictive pattern: VC, MVV.
6. ECG and echocardiography: for cases complicated with pulmonary hypertension and corpulmonale.
7. Other special investigations:
- Analysis of sodium chloride in the sweat in cystic fibrosis.
- Bronchoscopy is indicated in cases of localized bronchiectasis for the possibility of foreign body aspiration or bronchial adenoma.
- Aortography for diagnosis of the sequestrated lobe.
- Immunoglobulin assay, AAT level, collagenic profile.
Differential Diagnosis
- Chronic bronchitis
- T.B.
- Lung abscess.
- • Other causes of haemoptysis.
Complications
- Fatal hemoptysis.
- Brain abscess.
- Respiratory failure.
- Corpulmonale.
- Amyloidosis.
Treatment
- Antibiotics: more than one is beneficial + anti anaerobes are important to control the infective episodes of such suppurative disease.
- Expectorants and mucolytics (as described in the treatment of COPD).
- Postural drainage.
- Bronchodilators if associated with bronchospasm.
- Management of massive hemoptysis which is a serious complication of bronchiectasis.
Massive hemoptysis is defined as coughing about 600ml or more of blood in a day. However, other references considered hemoptysis to be massive if > 200 ml/day is coughed moderate if >20 ml to< 200ml/day, and mild if it is less than 20ml/day.
Important items in the management of hemoptysis include
- Reassurance.
- anti-shock measures, and blood transfusion (emergency treatment).
- Anti-shock on or side of bleeding is known, placing the bleeding lung in a dependent position may prevent blood spillage into the non-bleeding lung.
- Cough sedatives only 30-60ml paracodeine to avoid respiratory center depression due to overdose.
- Endobronchial tamponade by the bronchoscope, Fogarty’s catheter or double lumen endotracheal tube (Carlens tube) which tube allows ventilation of the good lung with simultaneous isolation and suctioning of the bleeding lung.
- Installation of local agents to control bleeding e.g. local coagulants, adrenaline or iced saline.
- Local cryotherapy, and electrocautery to the bleeding area.
- Bronchial artery embolization is carried out by injection gel foam. Before bronchial artery embolization, be sure that the spinal arteries are not abnormally arising from that artery otherwise infarction of the spinal cord with subsequent paraplegia will occur.
- Lastly, surgical resection is another important line of management for this serious condition.
6. Surgery in the form of surgical resection of the bronchiectasis lobe may be indicated in localized bronchiectasis or uncontrolled massive hemoptysis or lobectomy or pneumonectomy.
However, it should be emphasized that the treatment of bronchiectasis is mainly medical.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Suppurative Lung Diseases, Stages of Lung Abscess, Does a lung abscess require surgery?
Tuberculosis symptoms, What causes TB disease? and Can TB be transmitted through saliva?
Inflammation of the lung parenchyma, What causes lung parenchyma?, Is lung parenchyma dangerous
Hospital-Acquired Pneumonia Symptoms and Treatment, What is the difference between HAP and VAP?
Pneumonia causes, types, treatment, Is pneumonia usually serious? and Is pneumonia contagious?
Chronic Obstructive Pulmonary Diseases Treatment, Types and Causes of COPD
Steps of Asthma Control, What is good control of asthma? and What is asthma management?
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax