Bronchial asthma symptoms, causes, treatment, What is the difference between asthma and bronchial?
Bronchial Asthma can make breathing difficult and trigger wheezing, coughing, and chest tightness, It is a chronic lung condition that causes airways to become inflamed and narrow.
Bronchial Asthma
Bronchial Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role, In susceptible individuals, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning.
These recurrent episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment, The inflammation also causes an associated increase in the existing bronchial hyper-responsiveness to a variety of stimuli.
Symptoms of asthma
Symptoms of asthma are Wheezing (a whistling sound when breathing), Coughing, especially at night or in the morning, Shortness of breath, Chest tightness, Feeling tired, or having trouble sleeping.
Triggers of asthma
There are many triggers: Allergens, such as pollen, dust mites, pet dander, and mold, Irritants, such as smoke, air pollution, strong odors, and cold air, Respiratory infections, such as colds and flu, Exercise, and Stress.
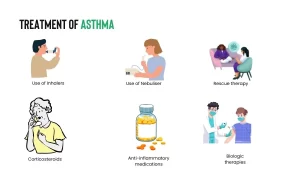
Asthma treatment
- Asthma treatment involves a combination of medications and lifestyle changes. These may include:
- Inhaled corticosteroids (ICS) can reduce inflammation in the airways.
- Short-acting beta-agonists (SABAs) relax the muscles in the airways, making it easier to breathe.
- Long-acting beta-agonists (LABAs) help prevent asthma attacks.
- Leukotriene modifiers can block the effects of leukotrienes, which are substances that can cause inflammation in the airways.
- Theophylline relaxes the muscles in the airways.
- Avoiding triggers can help prevent asthma attacks.
Pathogenesis of asthma
The airway Inflammation has a central role in the pathogenesis of asthma, Inflammation involves a complex interaction of inflammatory cells (e.g. mast cell, CD4 T lymphocyte, eosinophil, and airway epithelial cell) and resident airway cells.
The triggers of asthma such as infection, allergens, and air pollution lead to the activation of mast cells and Th2 cells in the airway. They in turn induce the production of mediators of inflammation such as histamine leukotrienes and cytokines.
These mediators result in the stimulation of mucous secretion and smooth muscle contraction, as well as differentiation & migration of eosinophils to the lung. On activation, the eosinophils release inflammatory mediators & enzymes that injure airway tissues, prolong eosinophil survival, and contribute to persistent airway inflammation.
The airway inflammation leads to the development of airway hyper-responsiveness, airflow limitation, respiratory symptoms, and disease chronicity. Chronic airway inflammation results in airway remodeling, which is defined as changes in the composition, content, and organization of the cellular and molecular constituents of the airway wall.
These permanent structural changes include:
- Epithelial detachment.
- Subepithelial fibrosis.
- Increased airway smooth muscle (ASM) mass.
- Goblet cell and mucus gland hyperplasia.
- Proliferation of blood vessels and airway edema
- Changes in the cartilage.
Risk factors that lead to asthma development
- Host factors: Genetic predisposition, atopy, gender.
- The environmental factors are Allergens, air pollution, respiratory infections, tobacco smoke, diet, and drugs (NSAIDs, aspirin, beta blockers).
Types of asthma
In Extrinsic Asthma: Atopic, Positive family history, Usually starts in childhood, High serum Ig E, Sputum eosinophilia, Positive skin test, Usually easy to control, Usually, allergen-induced.
In Intrinsic Asthma: Non-atopic, Negative family history, Starts at any age, Negative skin test, Usually difficult to control, Usually, non-allergen induced, Nocturnal asthma, and Exercise-induced asthma.
Special forms of asthma
- Nocturnal asthma – Occupational asthma.
- Exercise-induced asthma – Aspirin-induced asthma.
- Steroid-resistant asthma – Cough-variant asthma.
- Asthma in pregnancy.
Clinical Picture
Typical symptoms of asthma include wheezes, breathlessness, cough, and sensation of chest tightness. These symptoms may occur for the first time at any age and may be episodic or persistent.
Patients with episodic asthma are usually asymptomatic between exacerbations, which occur during viral respiratory tract infections or after exposure to allergens, Symptoms worsen at night and may occur or worsen in seasonal pattern, improve with anti-asthma therapy. This pattern is commonly seen in children or young adults who are atopic.
In other patients, the clinical pattern is of persistent asthma with chronic wheezing and breathlessness. This pattern is more common in older patients with adult-onset asthma who are non-atopic and typify intrinsic asthma.
Common triggers for asthmatic symptoms include exposure to allergens (pets, dust mites, Cockroach, molds, and pollens), exercise, weather changes (cold and dry weather, high humidity) viral infections, Tobacco smoke, and emotions.
Wheezing is usually expiratory but may be present during inspiration. Wheezing may be absent in case of very mild or very severe airway obstruction. Severe airway obstruction leads to marked limitation of airflow (silent chest). Signs of hyperinflation and diminished breath and heart sounds may be present during an acute exacerbation.
Asthma diagnosis
Diagnosis of asthma depends on:
- History and pattern of symptoms and physical examination
- Physiological assessment.
A. Measurement of lung function using spirometry provides an assessment of the severity, reversibility, and variability of airflow limitation, and helps to confirm the diagnosis of asthma.
- Pulmonary function tests: Obstructive pattern during the attack, normal in between attacks (except in moderate & severe persistent asthma).
- Reversibility test: If FEV1 increased by 12% + at least 200 ml (absolute value), after inhalation of SABA, indicates reversible airflow limitation consistent with asthma.
- PEFR Variability test: diurnal PEFR variability >20% suggests diagnosis of asthma.
B. “Broncho-provocation test”: using methacholine, histamine, adenosine, exercise, etc. to induce bronchospasm in patients with normal lung functions.
3. Skin Prick test: to assess the allergic status.
4. Laboratory tests:
- Peripheral blood eosinophilia > 4%.
- Sputum eosinophilia.
- Serum IgE.
5. ABG measurement: for staging an acute severe attack.
6. Radiological: Chest X-ray is normal in bronchial asthma except if persistent asthma or during an acute attack, there will be hyperinflation. Where it could be abnormal if complications are detected e.g., pneumothorax pneumomediastinum due to mucus plugs.
7. Electrocardiogram (ECG): ECG is usually normal but during the attack, there may be arrhythmias or sinus tachycardia.
Differential Diagnosis
“Not every wheezer is asthmatic”
- COPD & other obstructive AW diseases (FB, tumor, LNs,…).
- Bronchitis.
- Bronchopneumonia.
- GERD
- Rhino-sinus disease
- CHF or pulmonary embolism.
- Upper Airway Obstruction (Vocal cord dysfunction).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax