Anemia in elderly causes, Myelodysplastic syndromes, Anemia of chronic disease and inflammation
The elderly is an important demographic population that is growing rapidly in the context of the increasing prevalence of anemia with age. While decreased hemoglobin levels were previously considered a normal consequence of aging, now there is evidence that Low Hb is a powerful prognostic marker for multiple adverse outcomes in the elderly.
Anemia in elderly
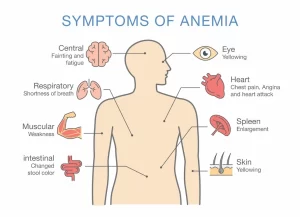
In older patients, anemia of any degree contributes significantly to morbidity, mortality, and hospitalization and has a significant effect on the quality of life, Anemia in the elderly has been associated with a higher incidence of cardiovascular disease, cognitive impairment, decreased physical performance and quality of life, and increased risk of falls and fractures.
Furthermore, the presence of anemia is significantly associated with longer hospital stays, and with an increased risk of mortality, in particular, mortality related to cardiovascular disease.
More importantly, anemia might be an early sign of a previously undiagnosed malignant disease, Despite its clinical importance, anemia in the elderly is under-recognized, and evidence-based guidelines on its management are lacking.
Anemia threshold
- According to hemoglobin (Hb) cut-off levels defined by the World Health Organization (WHO) (<12 g/dL for females, <13 g/dL for males).
- Anemia is present in 10% of women and 11% of men over the age of 65, increasing to 20% of women and 26% of men over 85.
- An even higher prevalence is seen in hospitalized patients, of whom approximately 40-50% are anemic.
Etiology of anemia in elderly
In elderly persons, the etiology of anemia differs sufficiently from the etiology in younger adults to warrant considering anemia in elderly persons as a distinct entity. Multiple conditions can lead to anemia in elderly persons. Moreover, the anemia may be multifactorial.
Iron deficiency anemia
- Identifying iron deficiency anemia in elderly persons is essential, and the condition can be corrected.
- More importantly, iron deficiency, particularly in elderly persons, often points to an underlying gastrointestinal pathology, including malignancy.
- Despite the importance of establishing a diagnosis, iron deficiency anemia represents only 15-23% of cases of anemia among the elderly.
Anemia of chronic disease and inflammation
- Anemia of chronic disease appears to be primarily related to inflammation, thus leading to the term anemia of chronic inflammation.
- Anemia of chronic inflammation is hyperproliferative anemia characterized by low serum iron and adequate to increased iron stores.
- Inflammatory markers implicated in anemia of chronic inflammation include TNF-alpha, IL-1, IFN-gamma, and IL-6.
- Inflammation inhibits erythropoiesis through a variety of mechanisms.
Renal insufficiency
- Chronic kidney disease is an important cause of anemia in elderly persons, especially considering that renal function declines with aging.
- Reduced renal EPO production is the primary factor leading to anemia in chronic kidney disease. Serum EPO levels are inappropriately low at a creatinine clearance of less than 40 mL/min.
- The precise degree of renal dysfunction sufficient to cause anemia remains controversial.
Nutrient deficiency
- vitamin B-12 deficiency is an uncommon cause of anemia in elderly persons.
- Folate deficiency is also uncommon, in part related to widespread vitamin supplementation.
- To the extent that such mineral deficiencies are reversible, they remain important to identify and treat.
Myelodysplastic syndromes
Myelodysplastic syndromes represent a heterogeneous group of disorders characterized by clonal hematopoiesis and peripheral blood cytopenias. They are more common in older adults and may present as an isolated anemia. In the elderly, anemia in conjunction with macrocytosis, thrombocytopenia, or neutropenia raises the suspicion of myelodysplastic syndrome.
Criteria of diagnosis of Myelodysplastic anemia
1. Chronic anemia is the major clinical finding, and bleeding tendency and fever are also observed.
2. Hematologic examination and bone marrow examination reveal all of the following:
- Cytopenia of 1-3 blood cell series in the peripheral blood.
- Dysplastic features of the blood cell morphology in the peripheral blood and bone marrow.
- 30% or fewer blasts in both the peripheral blood and bone marrow.
3. There is no other disease causative of cytopenia: Other causative diseases include leukemia, aplastic anemia, PNH, myelofibrosis, ITP, megaloblastic anemia, bone marrow metastasis of cancer, malignant lymphoma, multiple myeloma, hypersplenism, SLE, hemophagocytic syndrome, infection, and drug-induced hematological disorder.
4. The presence of the following findings increases the certainty of diagnosis.
- Normocellular or hypercellular bone marrow.
- Chromosomal abnormality of bone marrow cells.
- Cytochemical abnormality of blood cells (ringed sideroblasts, PAS-positive erythroblasts, peroxidase-negative neutrophils, decreased NAP score).
5. When making a diagnosis, myelodysplastic syndrome is suspected by agreement with items 1 and 2, other diseases are excluded by agreement with item 3, and the diagnosis is made more certain by agreement with item 4.
Unexplained Anemia
- Accounts for approximately one-third of all anemias in the elderly.
- Represents primarily a diagnosis of exclusion, unclassifiable by currently available methods.
- Potential explanations for the anemia have included low testosterone, occult inflammation, reduced hematopoietic reserve with advancing age, and inappropriately low serum EPO levels.
- This anemia is typically associated with a low serum EPO level for the degree of anemia. The EPO level usually falls within the normal reference range. However, this finding is abnormal, because serum EPO should rise with declining Hb values.
- Elevated hepcidin levels have been detected in UA, suggesting that inflammatory processes might contribute to anemia in the elderly, involving mechanisms similar to those encountered in ACD.
Approach to the elderly patient with anemia
History and Physical Examination
- Previous blood counts: help the clinician to DD acute blood loss as opposed to the more common slow decline in Hb over time.
- Transfusion history: alert the clinician to a chronic problem.
- Medical history: Recent hospitalization, Recent surgery, Diseases that frequently cause anemia.
- Nutritional history, alcohol overuse.
- Racial background: thalassemia trait.
- Symptoms: relate to the rapidity of the anemia, the depth of the Hb fall, and concomitant medical conditions, The nonspecific nature of anemia-related symptoms which are mistakenly attributed to aging or other medications poses a major challenge, Nevertheless, a detailed history often identifies the presence of anemia-related symptoms. Blood loss should be directly inquired about (eg, melena, hematuria, hemoptysis, hematemesis).
- The physical examination may uncover an anemia etiology, signs related to the anemia, or both, Thus, the examination must be comprehensive.
Investigations
- IDA: iron panel, fecal occult blood test, endoscopy
- Levels of vitamin B12, folate, Homocysteine.
- Others: thyroid function tests, liver tests, renal panels.
- Bone marrow aspirate and biopsy are used when a primary marrow disease (eg, MDS, aplastic anemia) is suspected.
- New parameters include plasma hepcidin, erythroferron and soluble hemojuvelin. This should lead to a better understanding of the pathophysiology and the role of hepcidin-targeted therapeutics.
Treatment
IDA: oral iron preparation, parenteral preparation, and blood transfusions should be reserved for the treatment of shock or hypoxia.
Balanced diet + Vitamin supplementation namely vitamin B12, folic acid
Considering the central role of hepcidin in the pathophysiology of anemia in the elderly, it is not surprising that a plethora of drugs manipulating the hepcidin pathway for therapeutic purposes have been developed with some of these agents already being applied in clinical studies.
Blood transfusion: Complications of blood transfusion led to the realization that it is better to allow the normal compensatory cardiovascular response to anemia to preserve oxygen transport in patients who were otherwise stable and did not have risk factors. Based on Level 1 evidence it is now generally agreed that a more restrictive transfusion practice is safe, with equivalent patient outcomes compared with transfusion practice to maintain hemoglobin levels above 10 g/dL.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Anemias causes, symptoms, features, diagnosis, and Types of Polycythemia
Functions and sources of Folic acid, Cobalamin (vitamin B12) and Vitamin K
Factors that help iron absorption, Daily iron requirements, and Abnormal iron levels
Red blood cells (Erythrocytes) structure & function, Myeloid tissue and Bone marrow
Hemoglobin structure, review, and Types of normal hemoglobin
Abnormal types of hemoglobin, Sickling of RBCs, Types, and causes of methemoglobinemia
Blood groups, Rh blood groups, Erythroblastosis fetalis, and the Importance of Rh factor