Advantages and Disadvantages of Using Interventional Radiology in Pain Management
Interventional radiology (IR) has become an increasingly valuable tool in pain management. By using imaging guidance (such as ultrasound, CT, or fluoroscopy), IR specialists can target sources of pain with high precision, often providing alternatives to more invasive surgical procedures.
What is the role of IR in pain management?
Pain management and interventional radiology (IR) intersect significantly in healthcare. Interventional radiologists use image-guided techniques to treat chronic and acute pain conditions, often offering minimally invasive alternatives to surgery.
Interventional radiology in pain management is a rapidly evolving field, providing effective, minimally invasive pain relief alternatives. For those with chronic pain or those not responding to conventional treatments, these procedures can significantly improve their quality of life.
Interventional radiology in pain management can be highly beneficial, particularly for patients who are not candidates for surgery or those seeking minimally invasive options for pain relief. IR works best as part of a multidisciplinary approach, combining pain relief with physical therapy, lifestyle modifications, and other treatments to achieve optimal outcomes.
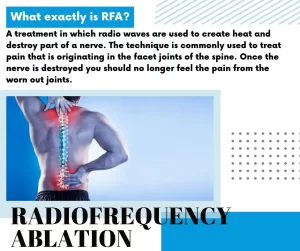
Nerve Blocks and Ablations provide relief from nerve pain by targeting and blocking pain pathways. Techniques like radiofrequency ablation, in which heat or cold disrupts nerve transmission, and neurolytic blocks are commonly used for chronic pain (e.g., spinal, cancer, and musculoskeletal pain). Benefits: Minimally invasive, usually with minimal recovery time.
Epidural Steroid Injections (ESI) reduce inflammation around nerves and are commonly used for back and neck pain. An anti-inflammatory steroid is injected near the spinal nerves, typically under X-ray guidance for precise delivery. Benefits: Offers potential for immediate relief, allowing patients to avoid or delay surgery.
Vertebroplasty and Kyphoplasty alleviate pain from vertebral compression fractures. Cement is injected into fractured vertebrae (vertebroplasty) or first a balloon creates space in the vertebrae before cement injection (kyphoplasty). Benefits: Minimally invasive and provides fast pain relief for osteoporosis-related fractures.
Sympathetic Nerve Blocks target sympathetic nerves for pain control in conditions like complex regional pain syndrome (CRPS). Injection of anesthetics around the nerves can interrupt pain signals, helping manage severe chronic pain. Benefits: Diagnostic and therapeutic; helps confirm the pain source and offer relief.
Spinal Cord Stimulation (SCS) treats chronic pain by disrupting pain signals sent to the brain. Electrodes are implanted near the spinal cord, and the device emits electrical pulses to alter pain perception. Benefits: Adjustable for each patient’s needs, providing long-term pain management.
Intra-articular Joint Injections treat arthritis or joint pain. IR-guided corticosteroids or hyaluronic acid injections directly into joints like the hip, knee, or shoulder. Benefits: Targets the pain source directly, providing a longer-lasting solution than systemic medications.
Conditions Commonly Treated with Interventional Pain Management
- Chronic lower back pain and sciatica.
- Cancer-related pain.
- Osteoarthritis and joint pain.
- Spinal fractures (due to osteoporosis or trauma).
- Peripheral neuropathies (nerve pain in the limbs).
- Complex regional pain syndrome (CRPS).
Advantages of Using Interventional Radiology in Pain Management
- Imaging guidance (CT, fluoroscopy, ultrasound) allows for accurate targeting. Procedures are usually done with small incisions or injections, leading to faster recovery. Many IR techniques provide effective pain relief, potentially reducing the need for narcotic medications.
- IR procedures are less invasive than traditional surgery, requiring only small incisions or needle punctures. This often results in less tissue trauma, faster recovery, and reduced scarring.
- The use of imaging guidance allows IR specialists to accurately target nerves, joints, or other pain sources, making treatment more effective with fewer side effects.
- Many IR procedures can be performed under local anesthesia, which lowers the risks associated with general anesthesia, especially for patients who may have other health complications.
- Minimally invasive techniques allow for faster recovery, often allowing patients to resume their daily activities sooner than they would with traditional surgical interventions. By providing long-lasting pain relief, IR treatments may reduce or eliminate the need for opioid medications, which can help decrease the risk of addiction and other opioid-related side effects.
- Interventional radiology offers a range of options for managing pain, including nerve blocks, joint injections, vertebroplasty for spinal fractures, and ablation techniques, making it a versatile choice for various pain conditions.
- IR can be especially beneficial for chronic pain patients who have not responded well to conventional treatments. Procedures like radiofrequency ablation (RFA) can provide longer-lasting relief than temporary pain medications.
Disadvantages of Interventional Radiology in Pain Management
- Although less invasive, IR procedures still carry risks, such as infection, bleeding, nerve damage, or unintended tissue injury, especially when working near sensitive structures.
- IR might not be effective for all types of pain, particularly those with complex or multifactorial causes. Some conditions may still require more traditional medical or surgical approaches.
- Some interventional radiology treatments, like nerve blocks, provide only temporary pain relief, requiring repeat procedures for ongoing pain management.
- Certain IR procedures, such as fluoroscopy-guided interventions, involve radiation exposure. Repeated exposure, especially for chronic conditions, could increase long-term health risks, although these risks are generally low with modern equipment.
- The effectiveness of IR procedures heavily relies on the expertise and experience of the radiologist. A lack of access to skilled IR practitioners in some areas may limit the availability of these treatments.
- Some interventional radiology treatments for pain management may not be fully covered by insurance, leading to high out-of-pocket costs for patients. Access to IR treatments may also be limited by geographical and institutional factors.
- Treatments of Interventional Radiology focus on symptom relief rather than addressing the underlying cause of pain, For some patients, a more comprehensive approach may still be needed to address the root cause of their pain fully.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Common procedures of Interventional Radiology and the best Interventional Radiologists
Interventional radiology types, Robotic endovascular systems advantages and disadvantages
Cone beam CT vs. Fan beam CT, CBCT advantages, disadvantages and uses
Magnetic Resonance Imaging (MRI) uses, advantages and disadvantages
Computed Tomography (CT) types, uses, advantages and disadvantages
Artificial intelligence in radiology decision support systems, Medical Imaging and Healthcare
Enlarged prostate symptoms, Prostatic artery embolization (PAE) importance and risks
Hepatic Artery Embolization, Importance and risks of Embolization therapy for Liver cancer
Thyroid nodules, Thyroid Fine Needle Aspiration Biopsy importance and risks
Uterine fibroid embolization risks, importance and Minimally invasive procedure specialists