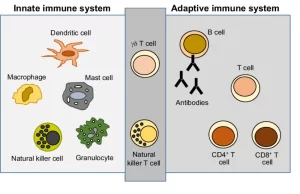
Adaptive immunity (Acquired immunity) types, Difference between Innate and Adaptive Immune responses
Acquired (adaptive or specific) immunity is a type of immunity that develops when a person’s immune system responds to a foreign substance or microorganism, or that occurs after a person receives antibodies from another source, Types of acquired immunity are adaptive and passive, Adaptive immunity occurs in response to being infected with or vaccinated against a microorganism.
Acquired (adaptive or specific) immunity
Acquired immunity is not present at birth. It is learned, when a person’s immune system encounters foreign invaders and recognizes nonself substances (antigens), the components of acquired immunity learn the best way to attack each antigen and begin to develop a memory for that antigen, Acquired immunity is called specific immunity because it tailors its attack to a specific antigen previously encountered, Its hallmarks are its ability to learn, adapt, and remember.
1. Active Immunity
In active immunity, the host cells learn to respond to foreign material, and the host actively produces the Abs, so they last longer than the readymade Abs given for immediate protection Its major disadvantage is its slow onset, especially the primary response.
a) Active Natural Immunity
It is the state of resistance built up in an individual following effective contact with foreign Ags (microorganisms or their products). The contact can be the result of clinical or subclinical infection.
b) Active Artificial Immunity
Through injection of killed or attenuated organisms toxoids, or recombinant peptides i.e., immunization by vaccines.
II. Passive Immunity
Immunity is temporary and it gives immediate protection because of receiving performed Abs.
a) Passive natural immunity
- IgG antibodies against some common infections pass trans-placentally from mother to the fetus.
- IgA Abs are also present in the colostrum and can be transmitted to the newborn via breastfeeding.
- Natural immunity protects the baby for 4-6 months only.
b) Passive artificial immunity
- The administration of preformed Abs, it is of greatest use when the illness is attributable to exotoxins, In such cases, the antibodies are called antitoxins (e.g. tetanus, and bolulism).
- Likewise preformed antibodies to rabies and hepatitis B viruses can be injected to neutralize the virus and thereby control viral replication.
The immunological response
It results from the introduction of an Ag into the body, The immune response may be:
1. Innate or non-specific: as inflammation and phagocytosis.
2. Adaptive or Specific:
- Humoral or antibody-mediated immunity is directed at extracellular pathogens & depends on B cells.
- Cell-mediated (or cellular) immunity depends on T cells to eliminate intracellular pathogens.
Specific or Adaptive Immune Response
Cells involved in the specific immune response:
1. Macrophages
They are phagocytic cells that are mainly concerned with processing and presentation of protein Ags to the lymphocytes and so they are called the antigen-presenting cells, They can also secrete cytokines e.g. interleukin-12, Other cells can also act as antigen-presenting cells such as Langerhans cells of the skin, dendritic cells, and B-lymphocytes.
2. T lymphocytes or T-cells
They originate from a stem cell in the bone marrow, and mature in the microenvironment of the thymus where they acquire a cluster of differentiation (CD) molecules, and differentiate into committed cells expressing specific T cell receptors (TCRs). T lymphocytes are important in defense against intracellular microbes, Several different subsets of T cells have been described, each with a distinct function, These include:
a. CD4 effector cells
- Th1 cells: Th1 cells secrete IFN-Y which amplifies Th1 response, activates macrophage, and enhances isotype switching to lgG. Also, Th1 cells produce IL 2 which acts on CD8-positive cells to enhance their proliferation and differentiation.
- Th2 cells: Th2 cells produce cytokines e.g., IL4, ILS, IL 13 which promote humoral immunity, IL4 causes B lymphocytes to isotype switch predominantly to IgE that are important in allergic responses, and ILS derives Isotype switching to IgA.
- Th17 cells: Th17 cells are of importance in the defense against fungal infection.
- T regulatory cells (T regs): CD4 T cells can become T (T regs) when they are exposed to TGF-β alone, T-reg cells function by suppressing T-cell responses.
b. CD8 positive T-cells
Which become differentiated into effector cytotoxic cells: cytotoxic T lymphocytes (CTLS), They kill infected host cells as virus-infected cells and tumor cells by the delivery of toxic granule content (perforin, granzymes, and granulysin).
3. B-lymphocytes or B-cells
Mature in the bone marrow and do not pass by the thymus, They are responsible for humoral immunity, All immature B cells carry IgM Immunoglobulin on their surface, These immunoglobulins serve as receptors (B-cell receptors (BCRS) for a specific antigen so that each B cell can respond to only one antigen or a closely related group of antigens, Mature human B-lymphocytes perform many functions including antibody secretion (after changing into plasma cells), Ag processing and presentation and cytokine secretion.
Adaptive immune responses develop in steps, consisting of antigen recognition, activation, proliferation, and differentiation of specific lymphocytes into effector and memory cells; elimination of the antigen; and decline of the response. The major events taking place in the specific immune response are:
Antigen processing and presentation
Proteins from exogenous antigens, such as bacteria, are internalized by the antigen-presenting cells (APC), Then undergo denaturation or partial proteolysis then the peptide fragments eventually become expressed on the surface of the APC (as peptide-MHC complex) to be recognized by the receptor on the surface of the specific T-helper cell.
Activation of the T-helper cell
Three kinds of signals are involved in the activation of T cells by APC:
- The first signal comes from the T cell receptor (TCR) on the T cell interacting with an MHC -peptide complex presented on the APC.
- The second signal (co-stimulation): is derived from the interaction of B7 costimulatory molecules on the APC with CD28 on the T cell.
- A third signal is delivered by the APCS: cytokines e.g., IL12.
During these events, these Th cells are able to proliferate and differentiate into effector T helper cells i.e., Th1, Th2, and Th17 cells.
Activation of B-cells: humoral or antibody-mediated immune response
There are two major pathways of B-cell activation:
1) T-cell-dependent activation: The full response of B cells to protein antigens requires help from T cells.
- B-cells recognize their specific antigen by surface membrane lg receptors, B cells also act as APCs-they ingest protein antigens, degrade them, and display peptides bound to class II MHC molecules for recognition by T helper cells.
- T helper cells express CD40 ligand (CD40L) and secrete cytokines, which work together to activate the B cells.
- Upon activation, B lymphocytes proliferate and then differentiate into antibody-secreting plasma cells.
- Also, B cells start to class switch to induce the production of antibodies of different classes (IgG, IgA, IgE).
- Helper T cells also stimulate the production of long-lived plasma cells and memory B cells.
2) T-cell-independent activation:
- Polysaccharides, lipids, and lipopolysaccharides are called T-cell-independent antigens because they induce antibody responses without T-cell help.
- Most T-independent antigens contain multiple identical epitopes that can crosslink many Ig receptors on a B cell providing signals that stimulate B cell responses.
- The response to T-independent antigens is generally weaker than other classes of antigens, It is dominated by IgM production, as class switching is dependent on cytokines released from T cells.
- The plasma cells generated are short-lived and there is no generation of memory cells.
Activation of T-cytotoxic cells
T-cytotoxic cells become activated when they recognize their antigen on the surface of a target cell, complexed with MHC class I molecule, and also by the effect of cytokines (e.g. IL 2) produced by Th1 cells. They differentiate into effector cytotoxic T lymphocytes (CTLS) that proceed to kill antigen-bearing target cells by their toxic granule content.
Some activated B and T-cells remain as Memory Cells that can respond to subsequent encounters with the same antigen, enabling a faster and more efficient response to re-infection with the same organism
The usual outcome of the immune response is the Elimination of the offending antigen. After the offending antigen elimination, the response is down-regulated by regulatory T cells to prevent unnecessary activation of lymphocytes and unregulated production of antibodies.
Interaction between Innate and Adaptive Immune responses
The innate and adaptive arms of the immune response do not operate independently of one another, “Phagocytic cells process and display antigen to facilitate stimulation of specific T- lymphocytes, “Macrophages secrete cytokines, which help trigger the initiation of specific immune responses, T lymphocytes produce cytokines which enhance the microbicidal activities of phagocytes.
By identifying PAMPS, microbial sensors not only initiate innate immune responses, but also activate adaptive immune responses These processes are bridges between innate immunity and adaptive immunity. Antibodies produced by plasma cells bind to pathogens and assist with phagocytosis and antibody-dependent cell-mediated cytotoxicity.
You can follow science online on Youtube from this link: Science online
You can download Science online application on google Play from this link: Science online Apps on Google Play
Immune response to infectious agents, Differences between natural & acquired immunity
Complement system function, Importance of MHC, Classical, Lectin, and alternative Pathways
Features and classification of viruses, Defective viruses & Viral vectors used for gene therapy
Cytokines function, use, definition, inflammation & side effects